Diabetes is a health condition that affects how the body turns food into energy. While there are several types of diabetes, type 2 diabetes is the most common form, distinguished by insulin resistance and often associated with lifestyle factors such as diet and physical activity. In type 2 diabetes, the body either resists the effects of insulin – a hormone that regulates the movement of sugar into cells – or doesn’t produce enough insulin to maintain normal glucose levels. This leads to elevated blood sugar levels, which can result in serious health complications if not managed effectively.
Magnesium is a fundamental mineral crucial for numerous biological functions, including nerve transmission, muscle contraction, and maintaining a healthy immune system. It plays a significant role in glucose metabolism and insulin action, making it a mineral of interest in diabetes. Despite its importance, magnesium deficiency is relatively common and can have significant health implications.
This article explores the complex connection between magnesium and diabetes, specifically focusing on how magnesium levels can affect developing and managing type 2 diabetes. By looking into current research and evidence, we will delve into the potential benefits of magnesium for people with diabetes and discuss recommendations for optimising magnesium intake.
Role of Magnesium in the Body
1. Biological Functions
Magnesium is a vital mineral for numerous biological processes within the human body. It plays a cofactor for over 600 enzymatic reactions, making it essential for various metabolic functions. These include:
- Enzyme Function: Magnesium is involved in energy production, as it helps form ATP (adenosine triphosphate), the primary energy carrier in cells. It also plays a role in the function of enzymes like hexokinase and phosphofructokinase, which are critical in the glycolytic pathway [1].
- Glucose Metabolism: Magnesium is integral to glucose metabolism and insulin action. It affects the activity of enzymes involved in carbohydrate metabolism, such as glucose-6-phosphatase and phosphoenolpyruvate carboxykinase in the liver [2].
- Muscle and Nerve Function: It is necessary for muscle contraction and relaxation, nerve signal transmission, and maintaining the structural integrity of proteins, nucleic acids, and mitochondria.
- Regulatory Functions: Magnesium modulates insulin signal transduction, cell proliferation, and transmembrane transport, including the movement of potassium and calcium ions.
2. Magnesium Sources
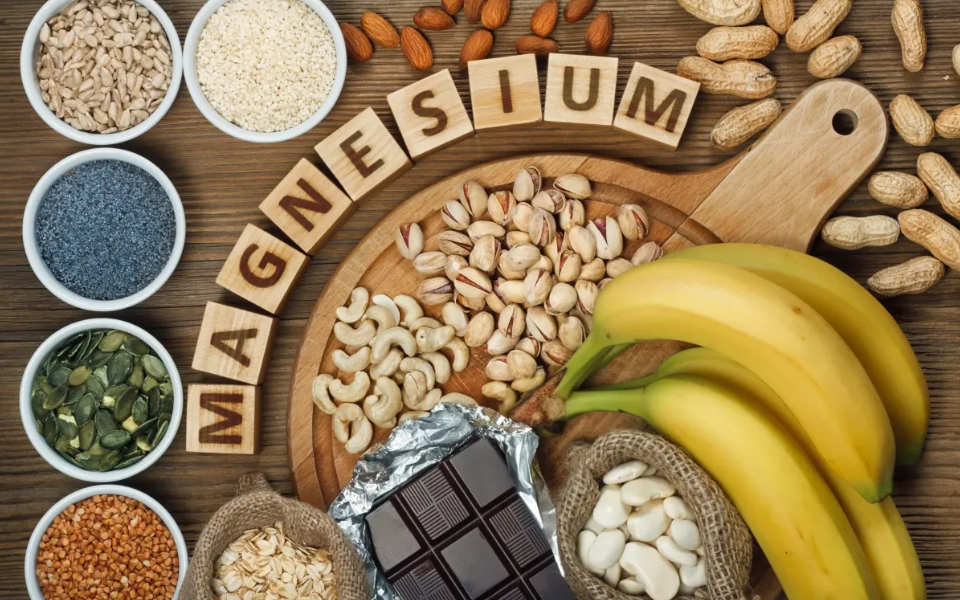
To maintain adequate magnesium levels, it is essential to include magnesium-rich foods in the diet. Some of the best dietary sources of magnesium include:
- Green Leafy Vegetables: Spinach and chard are mainly high in magnesium [3].
- Nuts and Seeds: Almonds, cashews, and pumpkin seeds are excellent sources.
- Whole Grains: Foods like quinoa and whole grain brown rice provide substantial amounts of magnesium.
- Legumes: Beans, lentils, and peanuts contribute to magnesium intake.
- Other Sources: Dark chocolate, avocados, and bananas also contain magnesium.
In addition to dietary sources, magnesium is available in various supplement forms, including magnesium citrate, magnesium oxide, and magnesium chloride. These supplements can help people who may not meet their magnesium needs through diet alone [4]. However, it’s important to consult with your medical doctor before starting any supplement regimen to ensure they are safe and useful.
What is the Connection between Magnesium and Diabetes?

1. Magnesium Deficiency in Diabetics
- Hypomagnesemia (low blood magnesium levels) is common in people with type 2 diabetes. Studies have shown that magnesium levels are lower in patients with diabetes compared to non-diabetic controls [5].
- The prevalence of magnesium deficiency in diabetics ranges from 13.5-47.7% in different studies [6].
2. Mechanisms of Magnesium Loss in Diabetics
Several factors contribute to magnesium deficiency in diabetics:
- Increased urinary excretion of magnesium due to osmotic diuresis from hyperglycaemia.
- Reduced tubular reabsorption of magnesium due to insulin resistance.
- Low dietary intake of magnesium-rich foods.
- Use of certain medications like loop and thiazide diuretics that promote magnesium wasting.
- Diabetic autonomic neuropathy affecting magnesium homeostasis.
3. Impact on Insulin Sensitivity
Magnesium plays a crucial role in insulin action and glucose metabolism:
- It acts as a cofactor for enzymes involved in glucose transport and insulin signalling [7].
- Intracellular magnesium is essential for the tyrosine kinase activity of the insulin receptor.
- Reduced intracellular magnesium concentrations result in defective tyrosine-kinase activity, postreceptorial impairment in insulin action, and worsening of insulin resistance in diabetic patients.
4. Studies Linking Magnesium and Insulin Sensitivity
- Multiple epidemiological studies have shown an inverse relationship between magnesium intake and the risk of developing type 2 diabetes [8].
- A meta-analysis found that for every 100 mg/day increase in magnesium intake, there was a 15% reduction in the risk of developing type 2 diabetes.
- Clinical trials have demonstrated that magnesium supplements can improve insulin sensitivity and glycemic control in people with diabetes or prediabetes, though results have been mixed.
The evidence strongly suggests that magnesium plays a vital role in glucose metabolism and insulin sensitivity. Magnesium deficiency is common in diabetics and may contribute to developing insulin resistance and type 2 diabetes.
Research-Based Insights
1. Epidemiological Studies
Multiple epidemiological studies have consistently shown an inverse link between magnesium intake and risk of developing type 2 diabetes:
- A meta-analysis of 13 prospective cohort studies involving 536,318 participants and 24,516 cases found a significant inverse association between magnesium intake and risk of type 2 diabetes (relative risk 0.78 [95% CI 0.73–0.84]) [9].
- Another meta-analysis of 7 studies with 286,668 participants found that a 100 mg/day increase in total magnesium intake decreased the risk of diabetes by 15% [10].
- A meta-analysis of 8 prospective cohort studies with 271,869 participants found a 23% lower relative risk of type 2 diabetes when comparing the highest vs. lowest magnesium intakes.
- The Nurses’ Health Study and Health Professionals Follow-up Study found an inverse association between magnesium intake and risk of type 2 diabetes in men and women over long-term follow-up [11].
2. Clinical Trials and Meta-Analyses
Clinical trials examining magnesium supplements have shown mixed results:
- A Brazilian trial with 128 poorly controlled diabetic patients found that magnesium supplements (500 mg/day or 1000 mg/day) for 30 days improved glycemic control.
- A small Mexican trial showed that magnesium supplements (300 mg/day) for 16 weeks reduced fasting glucose and HbA1c in diabetics with hypomagnesemia.
- However, another trial found no effect of magnesium supplements (369 mg/day) on glycemic control in diabetic patients taking insulin.
Meta-analyses have provided further insights:
- A dose-response meta-analysis found that for every 100 mg/day increase in magnesium intake, there was a 14% reduction in diabetes risk.
- The inverse association between magnesium intake and diabetes risk was stronger in overweight (BMI ≥25 kg/m2) individuals compared to those with normal weight.
- A meta-analysis of prospective studies found that higher magnesium intake was associated with a lower risk of progressing from prediabetes to diabetes [12].
The epidemiological evidence consistently shows an inverse relationship between magnesium intake and diabetes risk.
Health Benefits of Magnesium Supplement
Based on the research evidence, magnesium supplements appear to offer several health benefits for glycemic control and overall health in people with diabetes:
1. Improving Glycemic Control
- Magnesium supplements have been shown to improve insulin sensitivity and reduce insulin resistance in people with type 2 diabetes. A meta-analysis found that magnesium supplements for 4 months or longer significantly improved the HOMA-IR index (a measure of insulin resistance) in diabetic and non-diabetic subjects [13].
- Studies have demonstrated that oral magnesium supplements can reduce fasting blood glucose levels in people with diabetes. One clinical trial found that 250 mg/day of elemental magnesium for 3 months significantly improved HbA1c levels from 8.32% to 7.96% in type 2 diabetes patients [14].
- Magnesium supplements may help improve C-peptide levels, which is an indicator of insulin production. A study reported that 250 mg/day of magnesium reduced C-peptide from 2.28 to 1.90 ng/mL after 3 months.
2. Other Health Benefits
- Magnesium supplements have been associated with reduced blood pressure in some studies, which is particularly beneficial for diabetics who are at higher risk of cardiovascular disease.
- There is evidence that adequate magnesium intake may help reduce inflammation in the body. Chronic low-grade inflammation is common in diabetes and contributes to complications.
- Magnesium plays a role in bone health and may help promote stronger bones, which is important as diabetes can increase the risk of osteoporosis.
- Some research suggests magnesium supplements may help reduce the frequency of migraine attacks, improve exercise performance, and potentially alleviate symptoms of anxiety and depression.
It’s important to note that while these benefits are promising, the effects can vary between individuals [15]. The optimal dose and duration of supplements may differ based on a person’s current magnesium status and overall health. As always, it’s recommended to consult with your medical doctor before starting any new supplement regimen, especially if you have diabetes or other chronic health conditions.
Key Challenges and Considerations
1. Inconsistent Study Results
The mixed results observed in magnesium supplement studies can be attributed to several factors:
- Study Design Variations: Different studies employ varying methodologies, durations, and doses of magnesium supplements, making direct comparisons challenging. Some studies may be too short to observe significant effects, while others might use suboptimal doses.
- Population Differences: The baseline magnesium status of study participants can significantly impact results. Studies involving magnesium-deficient people are more likely to show positive effects compared to those with adequate magnesium levels [16].
- Magnesium Formulations: The bioavailability of magnesium varies depending on the form used (e.g., magnesium oxide vs. magnesium citrate). Some studies may use forms with lower bioavailability, potentially leading to less pronounced effects [17].
- Confounding Factors: Dietary habits, physical activity levels, and concurrent medications can affect magnesium metabolism and study outcomes. These factors are not always adequately controlled for in all studies.
- Measurement Techniques: The lack of standardised, reliable methods for assessing magnesium status contributes to inconsistencies across studies. Serum magnesium levels, often used as a marker, may not accurately reflect total body magnesium stores.
2. Safety and Doses
Recommended Dietary Allowances (RDAs) for magnesium vary by age and sex:
- Adult men: 400-420 mg/day
- Adult women: 310-320 mg/day (350-360 mg/day during pregnancy)
Regarding safety and potential side effects of excessive intake:
- Upper Intake Level: The tolerable upper intake level for magnesium supplements is 350 mg/day for adults. This does not include magnesium from food sources.
- Gastrointestinal Effects: The most common side effect of excessive magnesium intake from supplements is diarrhoea. Other gastrointestinal symptoms may include nausea and abdominal cramping.
- Drug Interactions: High doses of magnesium can interfere with the absorption of certain medications, including antibiotics and bisphosphonates.
- Renal Considerations: People with impaired kidney function are at higher risk of magnesium toxicity and should consult a healthcare provider before taking supplements.
- Hypermagnesemia: While rare in individuals with normal kidney function, very high doses of magnesium can lead to hypermagnesemia, potentially causing serious side effects such as low blood pressure, confusion, and cardiac arrhythmias.
It’s important to note that magnesium from dietary sources is generally safe and does not pose a risk of overdose due to the body’s ability to regulate absorption and excretion. However, when considering supplementation, it’s advisable to consult with your medical doctor to determine the appropriate doses and monitor for side effects or interactions with existing medications.
Practical Tips and Best Practices
Here are some practical recommendations for increasing magnesium intake:
1. Dietary Guidelines
To increase magnesium intake through diet, focus on combining the following foods:
- Legumes, nuts, and seeds: These are excellent sources of magnesium. Include foods like beans, lentils, almonds, cashews, and pumpkin seeds in your diet.
- Whole grains: Choose whole grain breads, cereals, and pasta over refined versions.
- Green leafy vegetables: Spinach and other dark green leafy vegetables are rich in magnesium.
- Dairy products: Milk and yoghurt contain magnesium.
- Other sources: Avocados, bananas, and dark chocolate also provide magnesium.
The Dietary Guidelines for Americans recommend a healthy dietary pattern that includes a selection of these magnesium-rich foods while limiting added sugars, unhealthy fats, and sodium.
2. Supplement Advice
When considering magnesium supplements:
- Consult your medical doctor: Before starting any supplement regimen, especially if you have a chronic health condition or take medications.
- Assess your need: Your healthcare provider can help determine if you’re at risk for magnesium deficiency based on your diet, health conditions, and medications.
- Choose the right form: Magnesium aspartate, citrate, lactate, and chloride are more easily absorbed forms of magnesium supplements.
- Mind the doses: The upper limit for magnesium supplements is 350 mg per day for adults. Excessive intake can cause side effects like diarrhoea and abdominal cramping.
- Consider timing: If you’re taking other medications, discuss proper timing with your healthcare provider, as magnesium can interact with certain drugs.
- Monitor for side effects: Be aware of potential gastrointestinal side effects and report any concerns to your healthcare provider.
- Reassess regularly: Regular check-ins with your healthcare provider can help ensure the supplement is necessary and effective.
Remember, while supplements can be helpful, it’s generally recommended to obtain nutrients primarily from a balanced diet. Magnesium supplements should be used to complement, not replace, a healthy eating pattern [18].
Conclusion
Throughout this article, we’ve explored the intricate link between magnesium and diabetes, highlighting several key points:
- Magnesium plays a crucial role in glucose metabolism and insulin sensitivity.
- People with type 2 diabetes often have lower magnesium levels, which can exacerbate insulin resistance.
- Epidemiological studies consistently show an inverse relationship between magnesium intake and diabetes risk.
- Clinical trials have demonstrated the potential benefits of magnesium supplements in improving glycemic control, though results have been mixed.
- Magnesium gives additional health benefits, including potential reductions in blood pressure and inflammation.
The importance of magnesium in diabetes management and prevention cannot be overstated. Adequate magnesium intake, whether through diet or supplement, may contribute significantly to better glucose control and reduced risk of developing type 2 diabetes. For people already diagnosed with diabetes, maintaining optimal magnesium levels could be an important component of their overall management strategy, potentially improving insulin sensitivity and reducing the risk of complications.
From a public health perspective, there’s a need for strategies to increase awareness about the importance of magnesium in overall health, specifically with diabetes. This could include:
- Integrating magnesium recommendations into diabetes prevention and management guidelines.
- Educating healthcare providers about the potential benefits of assessing and addressing magnesium status in patients at risk for or diagnosed with diabetes.
- Developing public health campaigns to promote the consumption of magnesium-rich foods as part of a balanced diet.
In conclusion, while magnesium is not a panacea for diabetes, its role in glucose metabolism and overall health makes it an important consideration in preventing and managing this widespread condition. As research continues to evolve, integrating magnesium awareness into clinical practice and public health strategies could contribute significantly to addressing the global diabetes epidemic.
Stay Informed & Inspired with Our Newsletter
Sign up for our newsletter to stay informed about the latest updates, episodes, helpful tips and strategies for diabetes management and holistic wellness.


