Lean diabetes is a form of diabetes in people with normal or low body mass index (BMI), unlike the typical type 2 diabetes associated with obesity. It presents unique challenges in diagnosis and management and is increasingly recognised worldwide, especially in developing countries and minority populations in developed nations.
This article explores lean diabetes, discussing its epidemiology, pathophysiology, clinical features, risk factors, complications, management, treatment strategies, and prevention, emphasising the need for personalised care and tailored public health strategies.
What is Lean Diabetes?
Lean Diabetes refers to a form of diabetes that occurs in people who are not overweight or obese. Unlike the more common type 2 diabetes, which is often associated with obesity and insulin resistance, lean diabetes typically affects people with a normal or low body mass index (BMI). This condition can present unique challenges in diagnosis and management due to its unusual characteristics.
Lean diabetes is less common than obesity-related type 2 diabetes but is increasingly recognised in various populations around the world. It is especially prevalent in certain developing countries and among minority populations in developed nations, such as the United States. The implication of lean diabetes lies in its contribution to the overall diabetes burden, highlighting the need for tailored public health strategies and clinical approaches. Understanding lean diabetes is crucial for addressing the full spectrum of the diabetes epidemic and ensuring that all affected people receive appropriate care.
Epidemiology
1. Prevalence Rates in Different Populations
Lean diabetes, though less common than obesity-related type 2 diabetes, is increasingly recognised in various populations worldwide. In a study conducted in northern India, out of 12,069 type 2 diabetes patients, 327 (2.7%) were classified as lean, indicating a notable presence of lean diabetes in this region [1]. In the United States, the prevalence of lean diabetes among adults increased from 4.5% in 2015 to 5.3% in 2020, representing a 17.8% increase. This rise was significant among Black, Hispanic, and female populations [2].
2. Demographic Characteristics
Lean diabetes tends to affect different demographic groups compared to obesity-related type 2 diabetes. In the U.S., lean diabetes showed a higher prevalence among minority populations, specifically African Americans and Latinos [3]. In addition, the condition was more prevalent among women, with a significant increase in prevalence rates from 2015 to 2020 [4]. In northern India, lean diabetes patients were generally younger compared to their overweight/obese counterparts.
3. Comparison with Obesity-Related Type 2 Diabetes
Lean diabetes differs significantly from obesity-related type 2 diabetes in several ways:
- Age: Lean diabetes patients are often younger than those with obesity-related type 2 diabetes.
- Gender: There is a male predominance in lean diabetes cases in the U.S., whereas obesity-related type 2 diabetes does not show such a strong gender bias.
- Ethnicity: Lean diabetes is more prevalent among minority populations, such as African Americans and Latinos, compared to obesity-related type 2 diabetes.
- Socioeconomic Status: Lean diabetes is often associated with lower socioeconomic status, which can influence access to healthcare and lifestyle factors contributing to the disease.
- Clinical Features: Lean diabetes patients tend to have more severe hyperglycaemia and may experience rapid beta-cell failure, leading to a higher prevalence of insulin use compared to obese diabetes patients.
These differences highlight the need for tailored approaches in diagnosing and managing lean diabetes, considering its unique epidemiological and demographic characteristics.
Pathophysiology
1. Impaired Insulin Secretion vs. Insulin Resistance
A complex interplay between impaired insulin secretion and insulin resistance characterises lean diabetes. Unlike obesity-related type 2 diabetes, where insulin resistance is the predominant feature, lean diabetes often involves a more significant impairment in insulin secretion. This impairment is primarily due to beta-cell dysfunction, which can occur even in the absence of significant insulin resistance [5]. The exact mechanisms behind this dysfunction are still under investigation, but it is clear that both genetic and environmental factors play a role.
2. Role of Beta-Cell Dysfunction
Beta-cell dysfunction is a critical factor in the development and progression of lean diabetes. Data from various studies, including the UKPDS, suggest that beta-cell dysfunction can begin well before the onset of hyperglycaemia and may be a primary driver of the disease. This dysfunction is characterised by a reduced first-phase insulin response, which is crucial for maintaining normal glucose levels. The feedback loop between insulin sensitivity and beta-cell function further complicates the picture, as individuals with lean diabetes may have normal or only slightly reduced insulin sensitivity, but their beta-cells fail to compensate adequately [7].
3. Concept of Sarcopenic Obesity
Sarcopenic obesity, a condition characterised by the coexistence of low muscle mass (sarcopenia) and excess fat, has been linked to an increased risk of type 2 diabetes, including lean diabetes. Sarcopenia can lead to altered glucose disposal and increased local inflammation, both of which contribute to the development of diabetes [6][8]. Studies have shown that individuals with sarcopenic obesity have a higher risk of developing type 2 diabetes compared to those with either condition alone. This increased risk is due to the combined effects of reduced muscle mass, which impairs glucose uptake, and excess fat, which exacerbates insulin resistance and inflammation [9].
4. Genetic, Autoimmune and Behavioural Factors
The pathophysiology of lean diabetes is influenced by a combination of genetic, autoimmune, and behavioural factors. Genetic predisposition plays a significant role, with multiple common and rare genetic variants contributing to the disease. Autoimmune factors may also be involved, as some individuals with lean diabetes exhibit markers of autoimmune activity, although this is less common than in type 1 diabetes. Behavioural factors, such as poor nutrition during fetal development and early childhood, can predispose people to lean diabetes by affecting beta-cell function and insulin sensitivity later in life. In addition, lifestyle factors such as physical inactivity and stress can exacerbate the condition.
In summary, lean diabetes is a multifaceted condition with a pathophysiology that involves impaired insulin secretion, beta-cell dysfunction, sarcopenic obesity, and a range of genetic, autoimmune, and behavioural factors. Understanding these mechanisms is crucial for developing effective prevention and treatment strategies tailored to this unique form of diabetes.
Clinical Features

1. Symptoms and Diagnostic Criteria
Lean type 2 diabetes mellitus (T2DM) presents with symptoms similar to those of classical type 2 diabetes, including:
- Polyuria (frequent urination)
- Polydipsia (excessive thirst)
- Unexplained weight loss
- Fatigue
- Blurred vision
The diagnostic criteria for lean T2DM are the same as for classical T2DM, which include:
- Fasting plasma glucose level ≥126 mg/dL (7.0 mmol/L)
- 2-hour plasma glucose level ≥200 mg/dL (11.1 mmol/L) during an oral glucose tolerance test (OGTT)
- Haemoglobin A1c (HbA1c) level ≥6.5%
- Random plasma glucose level ≥200 mg/dL (11.1 mmol/L) in a patient with classic symptoms of hyperglycaemia or hyperglycaemic crisis [10][11].
2. Differences from Classical Type 2 Diabetes
Lean T2DM differs from classical, obesity-related T2DM in several key aspects:
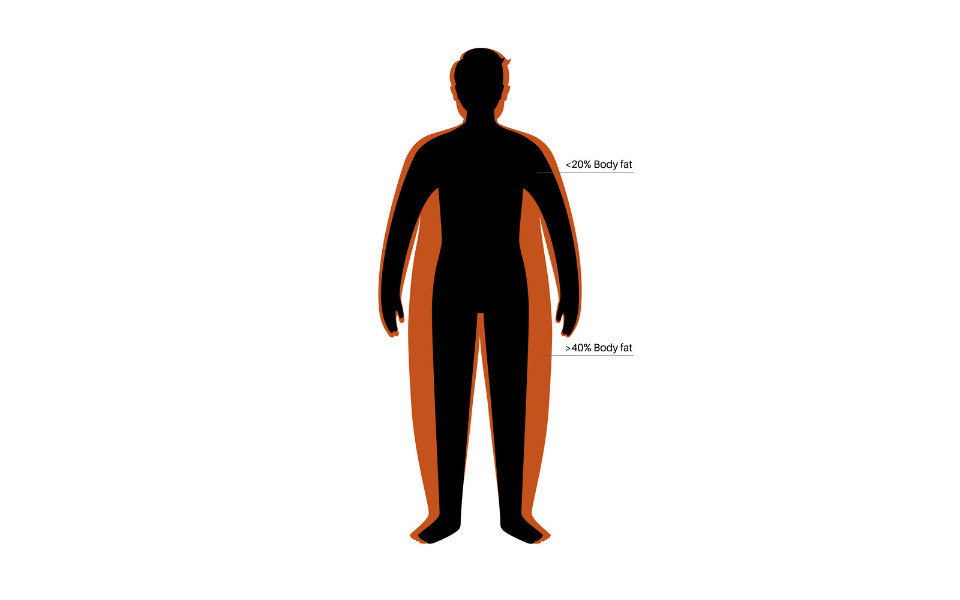
- Body Mass Index (BMI): Lean T2DM patients have a BMI <25 kg/m², whereas classical T2DM patients typically have a higher BMI.
- Insulin Secretion and Resistance: Lean T2DM is often characterised by more significant beta-cell dysfunction and less asserted insulin resistance compared to classical T2DM. This means that lean T2DM patients may have a more severe impairment in insulin secretion [12].Age of Onset: Lean T2DM can occur at a younger age compared to classical T2DM, which is more common in middle-aged and older adults.
- Autoimmune Markers: Lean T2DM patients generally lack autoimmune markers that are present in latent autoimmune diabetes in adults (LADA), distinguishing them from autoimmune forms of diabetes.
3. Metabolic Profile
The metabolic profile of lean T2DM patients includes several distinct features:
- Lipid Abnormalities: Lean T2DM patients often exhibit an atherogenic lipid profile, characterised by low levels of high-density lipoprotein (HDL) cholesterol and high levels of very-low-density lipoprotein (VLDL) cholesterol and triglycerides.
- Absence of Ketosis: Unlike type 1 diabetes, lean T2DM patients typically do not present with ketosis, as they still have some endogenous insulin production.Glucose Homeostasis: Lean T2DM patients may have impaired glucose sensing and beta-cell dysfunction, leading to poor glucose homeostasis despite normal or slightly reduced insulin sensitivity.
- Microvascular Complications: Lean T2DM patients are more prone to microvascular complications such as peripheral neuropathy, retinopathy, and nephropathy compared to macrovascular complications.
Lean T2DM is a distinct clinical entity with unique symptoms, diagnostic criteria, and metabolic profiles that differentiate it from classical, obesity-related T2DM. Understanding these differences is crucial for effective diagnosis and management of lean T2DM.
Risk Factors
1. Childhood Malnutrition
Studies in developing countries have shown that a history of childhood malnutrition is a risk factor for lean T2DM. Malnutrition during early life can affect beta-cell function and insulin sensitivity later in adulthood, predisposing individuals to diabetes.
2. Poor Socioeconomic Status
Lean T2DM is often associated with poor socioeconomic status, specifically in developing countries. Low socioeconomic status can influence access to healthcare, nutrition, and lifestyle factors contributing to the development of diabetes.
3. Sedentary Lifestyle
Physical inactivity is a significant risk factor for lean T2DM [13]. A sedentary lifestyle can alter metabolism and contribute to insulin resistance, increasing the risk of developing diabetes, even in non-obese individuals.
4. Stress and Tension
Chronic stress and tension can increase the risk of lean T2DM [14]. Stress triggers the release of cortisol, which can impair glucose metabolism and contribute to the development of diabetes.
5. Family History and Genetic Predisposition
Genetic susceptibility plays a role in developing lean T2DM [15]. People with a family history of diabetes, specifically lean T2DM, have an increased risk of developing the condition due to shared genetic and environmental factors within families.
In addition, the search results highlight other risk factors for lean T2DM, including:
- Alcohol Consumption: Consuming two or more alcoholic units per day (≥16 g/day) significantly increases the risk of lean T2DM.
- Fatty Liver Disease: Non-alcoholic fatty liver disease (NAFLD) is associated with an increased risk of developing lean T2DM.
- Diet: Diets high in sugar and unhealthy fats can contribute to the development of lean T2DM.
It is important to note that lean T2DM is a multifactorial condition, and the interplay of genetic, environmental, and behavioural factors contributes to its development and progression.
Complications
Key complications associated with lean type 2 diabetes mellitus (T2DM) include:
1. Cardiovascular Events (e.g., heart attacks)
Lean T2DM patients are at an increased risk of developing cardiovascular consequences, such as heart attacks, compared to obese T2DM patients. Despite having a normal or low BMI, individuals with lean T2DM often exhibit an atherogenic lipid profile characterised by low HDL cholesterol and high triglyceride levels, which can contribute to the development of cardiovascular disease [16].
2. Non-alcoholic Fatty Liver Disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD) is a common complication associated with lean T2DM. Even in the absence of obesity, people with lean T2DM may accumulate excess fat in the liver, leading to NAFLD. This condition can further exacerbate insulin resistance and increase the risk of developing other metabolic disorders [17].
3. Increased Mortality Rates Compared to Obese Diabetic Patients
Several studies have suggested that lean T2DM patients may have higher mortality rates compared to obese T2DM patients. The underlying reasons for this increased mortality are not fully understood, but it is hypothesised that the more severe impairment in insulin secretion and beta-cell dysfunction observed in lean T2DM patients may contribute to this increased risk.
In addition to the above complications, the search results also highlight other potential complications associated with lean T2DM, including:
- Microvascular Complications: Lean T2DM patients are more prone to microvascular complications such as peripheral neuropathy, retinopathy, and nephropathy compared to macrovascular complications.
- Rapid Progression: Lean T2DM patients may experience a more rapid progression of the disease, with early failure to respond to oral hypoglycaemic agents and a higher likelihood of requiring insulin therapy.
It is important to note that while lean T2DM patients may not exhibit the typical risk factors associated with obesity, they are still at risk for developing various complications related to diabetes. Early identification and appropriate management of lean T2DM are crucial to prevent or delay the onset of these complications.
Management and Treatment
1. Importance of Early Diagnosis
Early diagnosis of lean T2DM is crucial for initiating appropriate treatment and preventing or delaying complications. Lean T2DM patients may experience a more rapid progression of the disease and early failure to respond to oral hypoglycaemic agents, necessitating insulin therapy [19]. Identifying the condition early allows for timely intervention and better management.
2. Role of Exercise and Diet
Lifestyle changes, including regular exercise and a healthy diet, play a fundamental role in managing lean T2DM. Exercise can improve insulin sensitivity and glucose control, while a balanced diet can help maintain a healthy weight and prevent further complications [20]. Research indicates that many people can induce remission of T2DM by losing weight, which promises to change the way diabetes is managed.
3. Use of Insulin Sensitisers and Other Medications
Insulin sensitisers, such as metformin and pioglitazone, are commonly used in treating lean T2DM. Metformin is typically the first-line medication, as it reduces insulin resistance and hepatic glucose production [22]. Pioglitazone, an insulin sensitiser from the thiazolidinedione class, may be specifically beneficial for lean T2DM patients, as it can improve insulin sensitivity and beta-cell function [18].
Other medications, such as glucagon-like peptide-1 (GLP-1) agonists like liraglutide, can also be used to improve insulin secretion and glucose control in lean T2DM patients. However, the choice of medication should be personalised based on the patient’s specific needs and response to treatment.
4. Challenges in Therapy due to Pathophysiological Heterogeneity
Lean T2DM is a heterogeneous condition, with varying degrees of insulin resistance and beta-cell dysfunction among patients. This heterogeneity poses challenges in therapy, as some patients may respond better to insulin sensitisers, while others may require medications that primarily target beta-cell function. In addition, the underlying pathophysiology may differ between lean and obese T2DM patients, requiring tailored treatment approaches.
5. Personalised Treatment Plans
Due to the heterogeneity of lean T2DM, personalised treatment plans are essential. Factors such as age, duration of diabetes, comorbidities, and the patient’s response to therapy should be considered when developing a treatment plan. A multimodal approach, combining lifestyle changes, antihypertensive therapy, lipid-lowering therapy, and antihyperglycemic therapy, may be necessary to address the various aspects of the condition and reduce the risk of complications.
It is important to note that while insulin therapy may be necessary in some cases, it should be used cautiously in lean T2DM patients due to the increased risk of hypoglycaemia [21]. Treatment strategies should aim to avoid hypoglycaemia and minimise the need for insulin therapy when possible.
Managing and treating lean T2DM requires a comprehensive approach that addresses the unique pathophysiology and challenges associated with this condition. Early diagnosis, lifestyle changes, appropriate medication selection, and personalised treatment plans are crucial for achieving optimal glycaemic control and reducing the risk of complications.
Prevention
1. Lifestyle Changes (e.g. regular exercise, healthy diet)
Lifestyle changes, including regular physical activity and a healthy diet, are crucial in preventing lean T2DM. Research has consistently shown that combined lifestyle interventions, such as diet, exercise, and sustained weight loss, can effectively reduce the risk of T2DM by about 50% [27].
For lean individuals at risk of T2DM, regular exercise can improve insulin sensitivity and glucose control. A balanced diet, rich in nutrients and low in unhealthy fats and sugars, can help maintain a healthy weight and prevent further complications [25].
2. Importance of Early Screening, Especially in High-Risk Populations
Early screening for lean T2DM is essential, particularly in high-risk populations such as minority groups, people with a family history of diabetes, and those from lower socioeconomic backgrounds [23][24]. Early identification allows for timely intervention and lifestyle changes to prevent or delay the onset of the disease.
3. Public Health Strategies to Address Socioeconomic Factors
Lean T2DM is often associated with lower socioeconomic status, which can influence access to healthcare, nutrition, and lifestyle factors contributing to the disease [26]. Public health strategies addressing socioeconomic gaps and improving access to preventive care, education, and resources are crucial in combating lean T2DM.
These strategies may include:
- Improving access to affordable and nutritious food options in underserved communities
- Promoting physical activity through the development of safe and accessible recreational spaces
- Providing education and support programs for lifestyle changes and disease prevention
- Addressing social determinants of health, such as poverty, education, and access to healthcare services
By implementing comprehensive public health strategies that target socioeconomic factors, high-risk populations can be better equipped to adopt healthy lifestyles and reduce their risk of developing lean T2DM.
It is important to note that while lifestyle changes and early screening are essential, genetic predisposition also plays a significant role in developing lean T2DM. Therefore, a multifaceted approach that combines lifestyle interventions, early screening, and addressing socioeconomic factors is necessary for effective prevention.
Conclusion
Lean type 2 diabetes mellitus (T2DM) is a distinct form of diabetes that affects individuals with a normal or low body mass index (BMI). Despite its lower prevalence compared to obesity-related T2DM, lean T2DM contributes significantly to the global diabetes burden, specifically in certain developing countries and minority populations.
The pathophysiology of lean T2DM is characterised by a complex interplay between impaired insulin secretion, beta-cell dysfunction, and insulin resistance, with genetic, autoimmune, and behavioural factors playing crucial roles. Clinically, lean T2DM patients may exhibit an atherogenic lipid profile, an increased risk of microvascular complications, and a more rapid progression of the disease.
Risk factors for lean T2DM include childhood malnutrition, poor socioeconomic status, sedentary lifestyle, stress, and genetic predisposition. Complications associated with lean T2DM include cardiovascular events, non-alcoholic fatty liver disease (NAFLD), and potentially higher mortality rates compared to obese diabetic patients.
Managing and treating lean T2DM involves early diagnosis, lifestyle changes (regular exercise and a healthy diet), insulin sensitisers and other medications, and personalised treatment plans tailored to the patient’s specific needs and pathophysiology.
While our understanding of lean T2DM has improved, further research is crucial to unravel the complex mechanisms underlying this condition and develop more effective prevention and treatment strategies. Ongoing research efforts should focus on:
- Identifying genetic and epigenetic factors contributing to lean T2DM
- Exploring the role of autoimmunity and inflammation in the pathogenesis of lean T2DM
- Investigating the impact of early-life factors, such as childhood malnutrition, on the development of lean T2DM
- Developing personalised treatment approaches based on the heterogeneity of lean T2DM pathophysiology
- Evaluating the long-term outcomes and mortality rates associated with lean T2DM
By advancing our knowledge in these areas, we can improve our ability to prevent, diagnose, and treat lean T2DM more effectively.
By working together and adopting a comprehensive approach, we can mitigate the impact of lean T2DM and ensure better health outcomes for all people affected by this form of diabetes.
Stay Informed & Inspired with Our Newsletter
Sign up for our newsletter to stay informed about the latest updates, episodes, helpful tips and strategies for diabetes management and holistic wellness.


