Understanding the Hidden Culprit Behind Insulin Resistance
Hyperinsulinemia is excess insulin circulating in the blood relative to the glucose level. It is often mistaken for diabetes or hyperglycaemia, but it is distinct in that it involves elevated insulin levels rather than elevated blood sugar levels.
While hyperinsulinemia is commonly associated with early-stage type 2 diabetes, it is not the cause of the condition but rather a symptom. In type 2 diabetes, the body’s cells become resistant to insulin, leading to increased insulin production by the pancreas. This is different from type 1 diabetes, where the body produces insufficient insulin due to impaired pancreatic beta-cell function [1].
The prevalence of hyperinsulinemia has been increasing significantly. Data from a study conducted between 1999 and 2018 showed an 18% increase in the age-adjusted prevalence of hyperinsulinemia among adults in the U.S. without diabetes. This rise highlights the growing public health concern associated with hyperinsulinemia and its related complications [2].
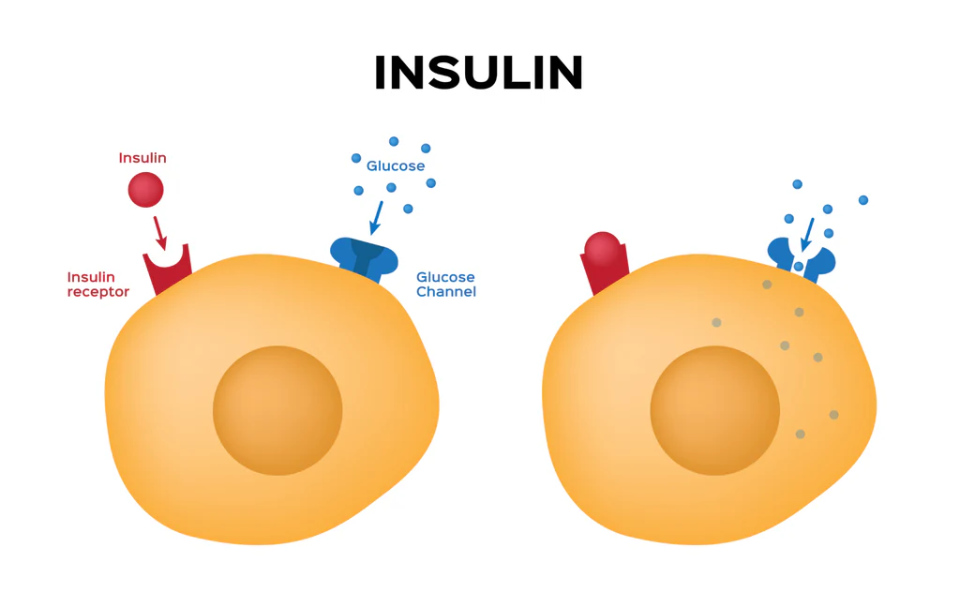
Insulin is a hormone produced by the pancreas that is vital for regulating blood glucose levels. It facilitates glucose uptake into cells, where it is used for energy or stored as glycogen. Insulin also influences fat and protein metabolism. When insulin levels are excessively high, it can lead to several adverse health outcomes, including:
- Metabolic Syndrome: A cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes.
- Cardiovascular Disease: High insulin levels can contribute to atherosclerosis, hypertension, and other cardiovascular issues.
- Certain Cancers: Elevated insulin levels have been linked to an increased risk of certain cancers, such as breast and colorectal cancer.
- Accelerated Ageing: Chronic hyperinsulinemia can lead to cellular damage and accelerated ageing processes.
Understanding hyperinsulinemia and its implications is crucial for developing effective prevention and management strategies to mitigate its impact on health.
Causes of Hyperinsulinemia
1. Insulin Resistance as Primary Driver
The primary cause of hyperinsulinemia is insulin resistance, a condition in which the body’s cells become less responsive to insulin. This condition leads to a compensatory increase in insulin production by the pancreas to overcome the resistance and maintain normal blood sugar levels. The following factors contribute to insulin resistance:
Obesity, Sedentary Lifestyle, and Poor Diet
- Excess body weight, specifically abdominal obesity, is strongly associated with insulin resistance and hyperinsulinemia [3].
- A sedentary lifestyle and lack of physical activity can worsen insulin resistance.
- A diet high in refined carbohydrates, unhealthy fats, and low in fibre can contribute to insulin resistance.
Genetic Factors
- Genetic predisposition plays a role in developing insulin resistance and hyperinsulinemia, with certain genetic variants increasing susceptibility.
- Family history and ethnicity can influence the risk of insulin resistance and related metabolic disorders.
2. Rare Causes
While insulin resistance is the primary driver, there are some rare causes of hyperinsulinemia:
Insulinoma Tumours
- Insulinomas are rare pancreatic tumours that secrete excessive amounts of insulin, leading to hyperinsulinemia and hypoglycaemia (low blood sugar) [4].
Nesidioblastosis
- Nesidioblastosis is a rare condition described by the abnormal proliferation of pancreatic islet cells, resulting in excessive insulin production and hyperinsulinemic hypoglycaemia [5].
- It is more commonly seen in infants but can also occur in adults, specifically after gastric bypass surgery.
Post-Gastric Surgery
- Hyperinsulinemia has been reported as a complication in some individuals after undergoing gastric bypass or other bariatric surgeries [6].
- The exact mechanisms are not fully understood but may involve changes in gut hormones, nutrient absorption, and pancreatic islet cell function.
While insulin resistance is the primary driver of hyperinsulinemia, these rare conditions can also lead to excessive insulin production and hyperinsulinemia through different mechanisms. Early recognition and appropriate management are crucial in addressing the underlying cause and preventing potential complications.
Symptoms and Diagnosis
Hyperinsulinemia often goes unnoticed in its early stages, as it can be asymptomatic initially. However, as the condition progresses, people may experience various symptoms:
Potential Symptoms
- Weight Gain: Excess insulin can promote fat storage, leading to weight gain, mainly around the abdomen.
- Increased Hunger and Cravings: High insulin levels can cause a drop in blood sugar levels, leading to increased hunger and cravings for sugary or carbohydrate-rich foods.
- Fatigue: Hyperinsulinemia can contribute to feelings of lethargy and low energy levels.
- Sugar Cravings: The body’s attempt to compensate for low blood sugar levels can lead to intense cravings for sugary foods.
It’s important to note that these symptoms are non-specific and can be associated with various other conditions.
Diagnostic Tests
To diagnose hyperinsulinemia, healthcare professionals may use the following tests:
- Insulin Levels: A blood test can measure insulin levels in the body. Elevated insulin levels, especially in the presence of normal or slightly elevated blood glucose levels, may indicate hyperinsulinemia.
- Glucose Tolerance Test: This test involves measuring blood glucose levels after consuming a glucose-rich drink. In people with hyperinsulinemia, insulin levels may be elevated, while glucose levels remain within the normal range or slightly elevated.
- C-Peptide Test: C-peptide is a byproduct of insulin production, and its levels can provide insight into the body’s insulin secretion. Elevated C-peptide levels, along with normal or slightly elevated blood glucose levels, can indicate hyperinsulinemia [7] [8] [9].
It’s important to note that a combination of these tests, along with a thorough medical history and physical examination, is often necessary to accurately diagnose hyperinsulinemia and rule out other potential causes of the symptoms.
Early detection and proper management of hyperinsulinemia are crucial to prevent or delay the development of associated health complications, such as metabolic syndrome, type 2 diabetes, and cardiovascular disease.
Health Risks of Hyperinsulinemia

Hyperinsulinemia, or excess insulin levels in the blood, is associated with several significant health risks. Longitudinal studies and research have highlighted the following potential consequences of chronic hyperinsulinemia:
1. Metabolic Syndrome
Hyperinsulinemia is a key component of metabolic syndrome, a cluster of conditions that includes abdominal obesity, high blood pressure, high triglycerides, low HDL cholesterol, and insulin resistance. Metabolic syndrome significantly increases the risk of developing type 2 diabetes and cardiovascular disease [10].
2. Type 2 Diabetes
Prolonged hyperinsulinemia can lead to the development of insulin resistance, a precursor to type 2 diabetes. As the body’s cells become less responsive to insulin, the pancreas compensates by producing even more insulin, eventually leading to beta-cell dysfunction and the onset of type 2 diabetes [11].
3. Cardiovascular Disease
Elevated insulin levels are associated with an increased risk of cardiovascular disease. Hyperinsulinemia can contribute to developing atherosclerosis, hypertension, and other cardiovascular issues through various mechanisms, including endothelial dysfunction, inflammation, and dyslipidaemia [12].
4. Certain Cancers
Several studies have linked hyperinsulinemia to an increased risk of certain types of cancer, including breast, colon, and pancreatic cancer. Insulin has been shown to have mitogenic effects, promoting cell proliferation and inhibiting apoptosis, which can contribute to tumour growth and progression [13].
5. Accelerated Ageing
Chronic hyperinsulinemia has been associated with accelerated ageing processes. Excess insulin can lead to cellular damage, oxidative stress, and inflammation, which can contribute to the development of age-related diseases and potentially shorten lifespan [14].
6. Evidence from Longitudinal Studies
Numerous longitudinal studies have provided evidence for the adverse health effects of hyperinsulinemia. For example, a prospective cohort study published in the International Journal of Cancer found that among non-obese people, hyperinsulinemia was associated with a significantly higher risk of cancer mortality. Another study published in Diabetes Care reported an association between hyperinsulinemia and an increased risk of fatal liver cancer [15].
It is important to note that while hyperinsulinemia is often associated with obesity and insulin resistance, it can also occur in non-obese people due to genetic factors or other underlying conditions. Early detection and management of hyperinsulinemia are crucial to mitigate the potential health risks and prevent the development of more severe metabolic disorders and associated complications.
Preventing and Treating Hyperinsulinemia
Hyperinsulinemia can be managed through a combination of lifestyle changes, medications, and, in rare cases, surgical intervention. The primary approach involves addressing the underlying causes, such as insulin resistance and obesity.
1. Lifestyle Interventions
Diet
- Adopting a low-carbohydrate, high-fibre diet can help regulate insulin levels and improve insulin sensitivity.
- Limiting refined carbohydrates, sugary foods, and beverages is recommended, as they can spike insulin levels.
- Increasing the intake of foods with a low glycemic index, such as non-starchy vegetables, lean proteins, and healthy fats, can help manage blood sugar and insulin levels.
Exercise and Weight Loss
- Regular physical activity, including aerobic exercise, anaerobic exercise and resistance training, can improve insulin sensitivity and promote weight loss, which can help reduce insulin resistance and hyperinsulinemia.
- Achieving and maintaining a healthy body weight through diet and exercise is crucial for managing hyperinsulinemia.
Stress Management
- Chronic stress can contribute to insulin resistance and make hyperinsulinemia worse.
- Combining stress-reducing techniques, such as meditation, yoga, or deep breathing exercises, may help improve insulin sensitivity and overall metabolic health.
2. Medications
Metformin
- Metformin is a commonly prescribed medication for people with insulin resistance and hyperinsulinemia.
- It works by reducing hepatic glucose production, increasing insulin sensitivity, and decreasing intestinal glucose absorption.
Other Diabetes Drugs
- In some cases, medications typically used to treat type 2 diabetes, such as GLP-1 agonists (e.g., liraglutide, semaglutide) or DPP-4 inhibitors (e.g., sitagliptin, linagliptin), may be prescribed to help manage hyperinsulinemia and improve insulin sensitivity.
3. Surgical Treatment for Insulinomas
In rare cases, hyperinsulinemia may be caused by an insulinoma, a tumour in the pancreas that produces excessive insulin. In such instances, surgical removal of the tumour (resection) may be recommended to cure the condition and restore normal insulin levels [16] [17] [18].
It’s important to note that the treatment approach for hyperinsulinemia should be tailored to the individual’s needs and underlying causes. A comprehensive evaluation by a healthcare professional is necessary to determine the most appropriate course of action.
The Insulin Resistance-Hyperinsulinemia Cycle
1. How Insulin Resistance Leads to Compensatory Hyperinsulinemia
Insulin resistance is a condition in which the body’s cells become less responsive to the effects of insulin, a hormone produced by the pancreas that regulates blood sugar levels. When insulin resistance occurs, the cells fail to efficiently utilise glucose from the bloodstream, leading to elevated blood sugar levels.
To compensate for this resistance, the pancreas responds by producing more insulin to overcome the resistance and facilitate glucose uptake by the cells. This increased insulin production results in hyperinsulinemia, or elevated insulin levels in the bloodstream.
2. How Hyperinsulinemia Worsens Insulin Resistance Over Time
While hyperinsulinemia initially serves as a compensatory mechanism, it can ultimately worsen insulin resistance over time, creating a vicious cycle:
- Chronic exposure to high insulin levels can lead to a phenomenon called “insulin desensitisation,” where the cells become less responsive to the effects of insulin, further increasing insulin resistance.
- Hyperinsulinemia can promote weight gain, specifically abdominal obesity, which is a major risk factor for insulin resistance. Excess body fat, especially around the abdomen, can contribute to inflammation and the release of substances that interfere with insulin signalling.
- Elevated insulin levels can also disrupt the normal metabolism of lipids, leading to an increase in free fatty acids in the bloodstream. High levels of free fatty acids can impair insulin signalling and glucose uptake in muscle and liver cells, further worsening insulin resistance.
- Hyperinsulinemia has been associated with developing other metabolic abnormalities, such as hypertension and dyslipidemia, which can further contribute to insulin resistance and increase the risk of cardiovascular disease.
3. Breaking the Vicious Cycle
To break the vicious cycle of insulin resistance and hyperinsulinemia, a multifaceted approach is often necessary:
- Lifestyle Changes: Adopting a healthy diet rich in fibre, lean proteins, and healthy fats, while limiting refined carbohydrates and added sugars, can help improve insulin sensitivity. Regular physical activity and weight loss (if overweight or obese) can also enhance insulin sensitivity and reduce insulin resistance.
- Medications: In some cases, medications such as metformin or insulin-sensitizing agents may be prescribed to improve insulin sensitivity and reduce the demand for insulin production.
- Addressing Underlying Conditions: If hyperinsulinemia is caused by an underlying condition, such as an insulinoma (insulin-producing tumour), appropriate treatment or surgical intervention may be necessary.
- Stress Management: Chronic stress can contribute to insulin resistance and exacerbate the cycle. Integrating stress-reducing techniques, such as meditation or yoga, may help improve insulin sensitivity.
By addressing insulin resistance through lifestyle changes, medications (if necessary), and managing underlying conditions, it is possible to break the vicious cycle of insulin resistance and hyperinsulinemia, reducing the risk of developing more severe metabolic disorders and associated complications [19] [20] [21] [22].
Societal and Economic Impacts

Hyperinsulinemia, if left unaddressed, can have significant societal and economic consequences, including:
1. Rising Healthcare Costs
Hyperinsulinemia is associated with an increased risk of developing various health conditions, such as metabolic syndrome, type 2 diabetes, cardiovascular disease, and certain cancers. Managing and treating these conditions can impose a substantial financial burden on healthcare systems and economies.
- According to a study published in the International Journal of Cancer, hyperinsulinemia was associated with a significantly higher risk of cancer mortality among non-obese individuals, potentially leading to increased healthcare expenditures for cancer treatment [23].
- The long-term complications of hyperinsulinemia and associated conditions, such as kidney disease and neuropathy, can further escalate healthcare costs due to the need for specialised treatments and hospitalisations.
2. Lost Productivity
Hyperinsulinemia and its related health complications can lead to decreased productivity and economic losses:
- People with hyperinsulinemia may experience fatigue, cognitive impairment, and other symptoms that can negatively impact their work performance and productivity.
- Health conditions associated with hyperinsulinemia, such as type 2 diabetes and cardiovascular disease, can result in increased absenteeism, presenteeism (reduced productivity while at work), and early retirement, leading to substantial productivity losses for employers and the economy [24].
3. Burden on Families and Caregivers
The impact of hyperinsulinemia extends beyond the individual, affecting families and caregivers:
- Individuals with severe complications of hyperinsulinemia may require assistance with daily activities, placing a significant burden on family members or caregivers who may need to take time off work or reduce their productivity.
- The emotional and psychological stress of caring for a loved one with a chronic condition can also take a toll on caregivers’ well-being and quality of life [25].
- The financial burden of medical expenses, lost income, and other costs associated with managing hyperinsulinemia and its complications can strain household budgets and contribute to economic hardship for families.
Addressing hyperinsulinemia through early detection, lifestyle interventions, and appropriate medical management can help mitigate these societal and economic impacts. Preventive measures, such as promoting healthy lifestyles and addressing risk factors like obesity and sedentary behaviour, can also play a crucial role in reducing the burden of hyperinsulinemia on individuals, families, and healthcare systems [26] [27].
Research Boundaries
Ongoing research is exploring several boundaries in the understanding and management of hyperinsulinemia, to develop more effective prevention and treatment strategies:
1. Genetics and Epigenetics
- Identifying genetic variants and epigenetic changes associated with an increased risk of developing hyperinsulinemia and insulin resistance.
- Understanding how these genetic and epigenetic factors influence insulin sensitivity, secretion, and signalling pathways.
- Exploring the potential for personalised medicine approaches based on an individual’s genetic and epigenetic profile.
2. Role of the Microbiome
- Investigating the relationship between the gut microbiome and insulin resistance/hyperinsulinemia.
- Examining how dysbiosis (imbalances in the gut microbiota) may contribute to metabolic dysfunction and impaired insulin sensitivity.
- Exploring the potential of microbiome-targeted interventions, such as prebiotics, probiotics, or faecal microbiota transplantation, in modulating insulin sensitivity and hyperinsulinemia.
3. Targeted Therapies
- Developing novel therapeutic agents that specifically target the underlying mechanisms of hyperinsulinemia and insulin resistance, such as insulin-sensitizing drugs or agents that modulate insulin secretion or clearance.
- Exploring the potential of repurposing existing medications for the management of hyperinsulinemia and related conditions.
- Investigating the use of combination therapies that address multiple aspects of the insulin resistance-hyperinsulinemia cycle.
4. Reversing Insulin Resistance
- Understanding the factors that contribute to reversing insulin resistance and hyperinsulinemia.
- Identifying the optimal timing and strategies for interventions intended to reverse insulin resistance and restore normal insulin sensitivity.
- Evaluating the long-term effects of reversing insulin resistance on preventing associated complications, such as type 2 diabetes, cardiovascular disease, and certain cancers [28] [29].
Ongoing research in these areas holds promise for improving our understanding of the complex mechanisms underlying hyperinsulinemia and insulin resistance, as well as developing more effective and personalised approaches to prevention and treatment.
Conclusion
Hyperinsulinemia, the condition described by excess levels of insulin in the blood, is a growing public health concern with far-reaching implications. As our understanding of this metabolic disorder deepens, it becomes increasingly clear that proactive measures and early intervention are crucial in mitigating its impact on individual and societal health.
Addressing the root causes of hyperinsulinemia, such as insulin resistance, obesity, and sedentary lifestyles, should be a priority. Promoting healthy dietary habits, regular physical activity, and maintaining a healthy body weight can go a long way in preventing the development of hyperinsulinemia and its associated complications.
Early detection through regular screening and diagnostic testing is also essential, as hyperinsulinemia can often be asymptomatic in its early stages. By identifying individuals at risk and implementing appropriate interventions, such as lifestyle changes or medications, the health condition progress can be slowed or even reversed.
Raising public awareness about hyperinsulinemia and its potential consequences is vital. Education campaigns and public health initiatives can empower people to make informed choices about their health and seek medical advice when necessary. By increasing awareness, we can promote a culture of prevention and early intervention, ultimately reducing the burden of hyperinsulinemia on individuals, families, and healthcare systems.
The research boundaries in hyperinsulinemia and insulin resistance are brimming with promise. Innovations in genetics, epigenetics, and microbiome research hold the potential to unlock new insights into the underlying mechanisms and pave the way for personalised and targeted therapies.
Furthermore, ongoing efforts to develop novel therapeutic agents and combination therapies offer hope for more effective management of hyperinsulinemia and its associated conditions. As our understanding of reversing insulin resistance deepens, we may witness a paradigm shift in the treatment of hyperinsulinemia, moving beyond symptom management towards restoring metabolic health.
In conclusion, hyperinsulinemia is a silent epidemic that demands our attention and collective action. By prioritising prevention, early intervention, public awareness, and continued research, we can pave the way towards a future where the burden of hyperinsulinemia is significantly reduced, and people can enjoy improved metabolic health and overall wellness.
Stay Informed & Inspired with Our Newsletter
Sign up for our newsletter to stay informed about the latest updates, episodes, helpful tips and strategies for diabetes management and holistic wellness.


