Blood sugar, also known as blood glucose, is a type of sugar that circulates in the bloodstream and serves as the primary source of energy for the body’s cells. Chemically, glucose is a six-carbon molecule with the formula C₆H₁₂O₆, and it is derived from digesting carbohydrates found in foods like bread, potatoes, and fruits. Once ingested, carbohydrates are broken down into simpler sugars, including glucose, which are then absorbed into the bloodstream through the small intestine.
Glucose is essential for the proper functioning of every organ system. It is the main energy substrate for cellular respiration, a process that converts glucose into adenosine triphosphate (ATP), the energy currency of the cell. This energy is crucial for various physiological functions, including muscle contraction, nerve impulse transmission, and the synthesis of essential molecules like hormones and cell membranes. The liver plays a critical role in regulating blood glucose levels by storing excess glucose as glycogen and releasing it back into the bloodstream when needed.
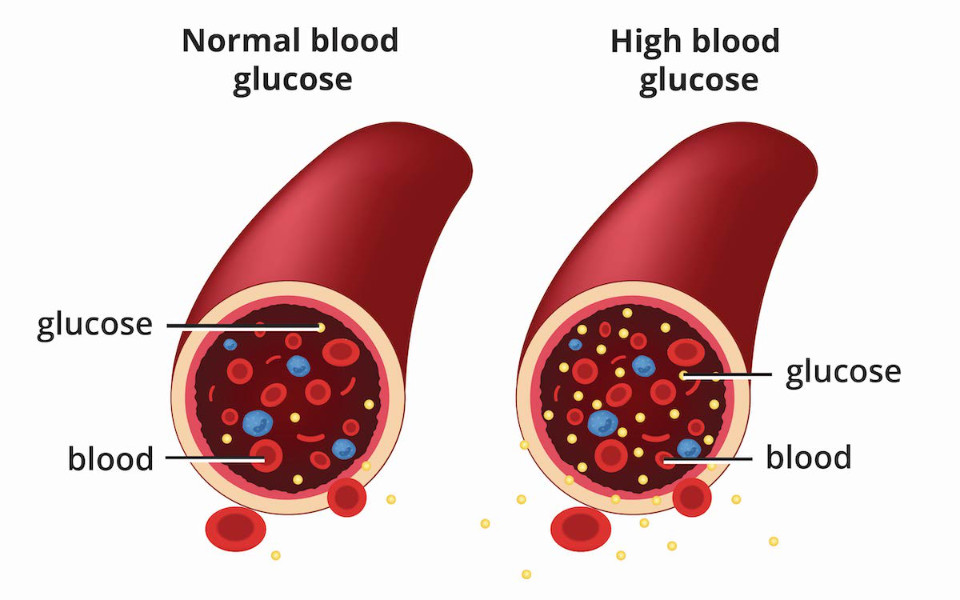
Diabetes is a health condition distinguished by elevated levels of blood glucose due to the body’s inability to produce sufficient insulin or effectively use the insulin it makes. Insulin is a hormone produced by the pancreas that facilitates glucose uptake into cells, lowering blood glucose levels.
There are three main types of diabetes:
- Type 1 Diabetes: An autoimmune condition where the body’s immune system attacks and destroys insulin-producing beta cells in the pancreas. This results in little to no insulin production, requiring lifelong insulin therapy.
- Type 2 Diabetes: A metabolic disorder described by insulin resistance, where the body’s cells do not respond effectively to insulin. Over time, the pancreas cannot produce enough insulin to maintain normal blood glucose levels. This type is often associated with obesity and lifestyle factors.
- Gestational Diabetes: A temporary form of diabetes that occurs during pregnancy. It involves insulin resistance and typically resolves after childbirth, although it increases the risk of developing type 2 diabetes later in life.
Maintaining blood glucose levels within a normal range is crucial for preventing the acute and chronic complications associated with diabetes. High blood glucose levels (hyperglycaemia) can lead to severe health issues, including cardiovascular disease, kidney damage, nerve damage, and vision problems. Conversely, low blood glucose levels (hypoglycaemia) can cause symptoms such as dizziness, confusion, and, in severe cases, loss of consciousness.
Effective diabetes management involves regular monitoring of blood glucose levels, following a balanced diet, regular physical activity, and, when necessary, medication or insulin therapy. By keeping blood glucose levels within target ranges, people with diabetes can significantly reduce the risk of complications and improve their overall quality of life.
Understanding Blood Sugar Levels
1. Blood Sugar (Glucose) and Its Role
Blood sugar, or glucose, is a simple sugar that is a crucial energy source for the body’s cells. It is obtained from the food we eat, particularly carbohydrates, which are broken down into glucose and other simple sugars during digestion. Once absorbed into the bloodstream, glucose is transported to cells throughout the body, where it is used to produce energy through cellular respiration. The brain, muscles, and other organs rely heavily on glucose to function properly.
The regulation of blood glucose levels is primarily managed by the hormone insulin, produced by the pancreas. Insulin facilitates the glucose uptake into cells, lowering blood glucose levels. When blood glucose levels drop, the pancreas releases glucagon, another hormone that signals the liver to release stored glucose, thereby raising blood glucose levels. This delicate balance ensures that the body has a consistent supply of energy.
2. How Blood Sugar Levels are Measured
Monitoring blood sugar levels is essential for managing diabetes and ensuring that blood glucose remains within a healthy range. There are several methods for measuring blood sugar levels:
a) Finger-Prick Tests
Finger-prick tests are the most common method for checking blood glucose levels. This method involves pricking the fingertip with a small, sterile lancet to obtain a drop of blood, which is then placed on a test strip inserted into a glucose meter. The meter measures the blood glucose level and displays the result within seconds. Finger-prick tests are typically used for daily monitoring and can be performed multiple times a day to track fluctuations in blood sugar levels.
b) Continuous Glucose Monitors (CGM)
Continuous glucose monitors (CGM) are advanced devices that provide real-time monitoring of blood glucose levels throughout the day and night. A small sensor is inserted under the skin, usually on the abdomen or arm, and it measures glucose levels in the interstitial fluid (the fluid between cells). The sensor transmits data to a receiver or smartphone app, allowing users to see their glucose levels and trends over time. CGMs can alert users to high or low blood glucose levels, helping them make timely changes to their diet, activity, or medication.
c) HbA1c Tests for Long-Term Monitoring
The HbA1c test, also known as the glycated haemoglobin, measures the average blood glucose levels over the past three months. Haemoglobin is a protein in red blood cells that carries oxygen, and when glucose binds to it, it forms glycated haemoglobin (HbA1c). The HbA1c test provides a percentage that reflects the average blood glucose level over time. For people with diabetes, an HbA1c level of less than 7% is generally considered a target, although specific goals may vary based on individual circumstances. This test is typically performed in a healthcare setting and is an important tool for assessing long-term blood glucose control.
Understanding and monitoring blood sugar levels are critical components of diabetes management. Blood glucose plays a vital role in providing energy to the body’s cells, and maintaining its levels within a healthy range is essential for preventing complications. Various methods, including finger-prick tests, continuous glucose monitors, and HbA1c tests, offer valuable insights into daily and long-term blood glucose control, enabling people with diabetes to make informed decisions about their health.
Types of Diabetes
1. Type 1 Diabetes
a) Autoimmune Nature and Insulin Dependency
Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This destruction results in little to no insulin production, a hormone essential for glucose uptake into cells [1]. As a result, people with type 1 diabetes are dependent on external insulin administration, either through injections or an insulin pump, to manage their blood sugar levels [2].
b) Impact on Blood Sugar Levels
Without insulin, glucose cannot enter the cells and remains in the bloodstream, leading to high blood sugar levels (hyperglycaemia). This condition requires careful monitoring and management to prevent acute complications like diabetic ketoacidosis and long-term complications such as cardiovascular disease and nerve damage [3].
2. Type 2 Diabetes
a) Insulin Resistance and Lifestyle Factors
Type 2 diabetes is distinguished by insulin resistance, where the body’s cells do not respond effectively to insulin. Over time, the pancreas cannot produce enough insulin to overcome this resistance, leading to elevated blood glucose levels [4]. Lifestyle factors such as obesity, physical inactivity, and poor diet significantly contribute to the development of insulin resistance and type 2 diabetes.
b) Risk Factors
Type 2 diabetes is the most common form of diabetes, accounting for the majority of diabetes cases worldwide. Risk factors include being overweight, having a sedentary lifestyle, being over the age of 45, and having a family history of diabetes. Ethnic background can also play a role, with higher prevalence rates observed in certain populations.
3. Gestational Diabetes
a) It Happens During Pregnancy
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased needs, leading to high blood sugar levels. It typically develops in the second or third trimester and usually resolves after childbirth [5].
b) Risks and Management Strategies
While most women with gestational diabetes have healthy pregnancies, the condition can increase the risk of complications such as having a larger baby, premature birth, and pre-eclampsia. It also raises the mother’s risk of developing type 2 diabetes later in life. Management strategies include monitoring blood sugar levels, adopting a healthy diet, engaging in regular physical activity, and, in some cases, using insulin or medication to control blood sugar levels. Early detection and management are crucial to minimising risks for both the mother and baby.
Blood Sugar Level Ranges
1. Normal vs. Diabetic Blood Sugar Level Ranges
Understanding the differences between normal and diabetic blood sugar levels is crucial for effective diabetes management [6]. Here are the general ranges:
- Normal Blood Sugar Levels:
- Fasting: 4.0 to 5.4 mmol/L (72 to 99 mg/dL)
- 2 hours after eating: Up to 7.8 mmol/L (140 mg/dL)
- Diabetic Blood Sugar Levels:
- Type 1 Diabetes:
- Before meals: 4 to 7 mmol/L
- 2 hours after meals: Under 9 mmol/L
- Type 2 Diabetes:
- Before meals: 4 to 7 mmol/L
- 2 hours after meals: Under 8.5 mmol/L
- Type 1 Diabetes:
2. Fasting and Postprandial Glucose Levels
- Fasting Glucose Levels:
- Normal: Less than 5.5 mmol/L (100 mg/dL)
- Prediabetes: 5.5 to 6.9 mmol/L (100 to 125 mg/dL)
- Diabetes: 7.0 mmol/L (126 mg/dL) or higher on two separate tests
- Postprandial (2 hours after eating) Glucose Levels:
- Normal: Less than 7.8 mmol/L (140 mg/dL)
- Prediabetes: 7.8 to 11.0 mmol/L (140 to 199 mg/dL)
- Diabetes: 11.1 mmol/L (200 mg/dL) or higher
3. Target Ranges for Different Types of Diabetes
- Adults with Type 1 Diabetes:
- Upon waking: 5 to 7 mmol/L
- Before meals: 4 to 7 mmol/L
- 90 minutes after meals: 5 to 9 mmol/L
- Children with Type 1 Diabetes:
- Before meals: 4 to 7 mmol/L
- 90 minutes after meals: 5 to 9 mmol/L
- Adults with Type 2 Diabetes:
- Before meals: 4 to 7 mmol/L
- 2 hours after meals: Under 8.5 mmol/L
- Pregnant Women with Diabetes:
- Fasting: Below 5.3 mmol/L
- 1 hour after meals: Below 7.8 mmol/L
- 2 hours after meals: Below 6.4 mmol/L
4. Maintaining Blood Sugar Levels to Prevent Complications
Maintaining blood sugar levels within the target range is essential for preventing both short-term and long-term complications associated with diabetes [7]. Consistently high blood sugar levels (hyperglycaemia) can lead to severe health issues, including:
- Cardiovascular Disease: Increased risk of heart attack and stroke due to damage to blood vessels and nerves.
- Neuropathy: Nerve damage that can cause pain, tingling, and loss of sensation, particularly in the extremities.
- Nephropathy: Kidney damage that can lead to kidney failure.
- Retinopathy: Damage to the blood vessels in the retina, leading to vision problems and potentially blindness.
- Foot Problems: Poor blood flow and nerve damage can lead to serious foot infections and even amputations.
Conversely, low blood sugar levels (hypoglycaemia) can cause immediate symptoms such as dizziness, confusion, and, in severe cases, loss of consciousness. Therefore, regular monitoring and proper management of blood sugar levels are critical to reducing the risk of these complications and improving the overall quality of life for people with diabetes.
Complications of High Blood Sugar (Hyperglycaemia)
1. Short-term Symptoms and Risks
When blood sugar levels are elevated, the body can experience a range of short-term symptoms and risks due to the inability of glucose to enter cells effectively. These include:
- Increased Thirst (Polydipsia): High blood sugar levels cause the body to pull fluid from tissues, leading to dehydration and increased thirst.
- Frequent Urination (Polyuria): The kidneys work to excrete excess glucose through urine, resulting in increased urination.
- Fatigue: Despite high glucose levels, cells are deprived of energy due to insufficient insulin or insulin resistance, leading to feelings of tiredness and fatigue.
If hyperglycaemia is not addressed, it can lead to more severe short-term conditions such as diabetic ketoacidosis (DKA) in type 1 diabetes, where the body starts breaking down fat for energy, producing ketones that can accumulate to dangerous levels in the blood.
2. Long-term Complications
Chronic hyperglycaemia, if left unmanaged, can lead to serious long-term complications that affect various organ systems:
- Cardiovascular Disease: High blood sugar levels can damage blood vessels and increase the risk of developing cardiovascular diseases, including coronary artery disease, heart attack, and stroke. People with diabetes are at a higher risk of developing these conditions due to the accelerated development of atherosclerosis (hardening of the arteries).
- Nerve Damage (Neuropathy): Prolonged high blood sugar can damage nerves, particularly in the legs and feet. This can lead to symptoms such as pain, tingling, numbness, and weakness. Peripheral neuropathy is common, but autonomic neuropathy can also affect the digestive system, heart, and other organs.
- Kidney Failure (Nephropathy): The kidneys filter waste from the blood, and high blood sugar levels can damage the delicate filtering system, leading to kidney disease or even kidney failure. Diabetic nephropathy is a leading cause of end-stage renal disease (ESRD).
- Vision Problems (Retinopathy): High blood sugar can damage the blood vessels in the retina, leading to diabetic retinopathy. This condition can result in vision impairment and, if untreated, can progress to blindness. Diabetes also increases the risk of other eye conditions, such as cataracts and glaucoma.
Managing blood sugar levels effectively through lifestyle changes, medication, and regular monitoring is crucial to reducing these risks and maintaining overall health. Early detection and intervention can significantly reduce the likelihood of developing these complications, improving the quality of life for people with diabetes.
Managing Blood Sugar Levels

1. Diet and Nutrition
a) Importance of Carbohydrate Control
Carbohydrates are the primary source of energy for the body and have the most significant impact on blood glucose levels. When consumed, carbohydrates are broken down into glucose, which enters the bloodstream. For people with diabetes, managing carbohydrate intake is crucial to maintaining stable blood sugar levels. This involves monitoring the type and amount of carbohydrates consumed, as different carbohydrates can affect blood sugar differently. Foods high in fibre, such as whole grains, fruits, and vegetables, can help slow glucose absorption, preventing spikes in blood sugar levels [8].
b) Impact of Diet on Blood Sugar Levels
Diet plays a critical role in managing diabetes. Consuming a balanced diet with appropriate portions of carbohydrates, proteins, and fats can help maintain blood sugar levels within target ranges. High intake of refined carbohydrates, sugary foods, and drinks can lead to rapid increases in blood sugar levels, while a diet rich in whole foods and low in processed sugars can promote better blood glucose control. Regular meals and snacks may help prevent blood sugar fluctuations.
2. Exercise and Physical Activity
a) Regular Exercise Role in Managing Blood Sugar
Regular physical activity helps manage blood sugar levels as it increases insulin sensitivity, allowing cells to use glucose more effectively. Exercise helps lower blood sugar levels and can have lasting effects for several hours after the activity. It also supports weight management and cardiovascular health, which are important for people with diabetes [9].
b) Recommendations for Different Diabetes Types
- Type 1 Diabetes: To prevent hypoglycaemia, people should monitor their blood sugar levels before, during, and after exercise. They may need to adjust their insulin doses or carbohydrate intake accordingly.
- Type 2 Diabetes: Regular aerobic and resistance exercises are recommended to improve insulin sensitivity and glucose metabolism. Activities such as walking, cycling, and strength training are helpful.
3. Medications and Insulin Therapy
a) Insulin and Non-Insulin Medications
For people with diabetes, especially type 1, insulin therapy is essential for managing blood sugar levels. Insulin can be administered through injections or an insulin pump. There are different types of insulin, including rapid-acting, short-acting, intermediate-acting, and long-acting, each with specific onset and duration times.
For type 2 diabetes, oral medications and non-insulin injectables may be prescribed to help the body use insulin more effectively or to increase insulin production. Common medications include metformin, sulfonylureas, and GLP-1 receptor agonists.
b) Adjusting Medication Based on Blood Sugar Monitoring
Regular monitoring of blood sugar levels is crucial for adjusting medication doses. This helps ensure that blood glucose remains within target ranges and reduces the risk of complications. Healthcare providers may adjust treatment plans based on blood glucose readings, HbA1c levels, and individual patient needs. Patients are encouraged to work closely with their healthcare provider to optimise their medication regimen and achieve better diabetes management outcomes [10].
Things to Consider About Blood Sugar
1. Prediabetes
a) Risk of Developing Type 2 Diabetes
Prediabetes is a condition described by blood sugar levels that are higher than normal but not yet high enough to be classified as type 2 diabetes. It represents an intermediate stage in the continuum from normal glucose regulation to diabetes. Prediabetes is often identified through laboratory measurements of fasting blood glucose (FBG), glycosylated haemoglobin (HbA1c), or 2-hour post-load blood glucose (2hBG) [11].
People with prediabetes are at a significantly increased risk of progressing to type 2 diabetes. According to research, the lifetime risk of progressing from prediabetes to overt diabetes is substantial, with estimates varying based on the definitions used by the American Diabetes Association (ADA) and the World Health Organization (WHO) [12]. For example, at age 45, the lifetime risk of developing diabetes for those with ADA-defined prediabetes is 57.5%, while it is 80.2% for those with WHO-defined prediabetes.
b) Strategies for Prevention
Preventing the progression from prediabetes to type 2 diabetes is possible through lifestyle changes. Key strategies include:
- Healthy Eating: Consuming a balanced diet rich in whole grains, fruits, vegetables, and lean proteins can help manage blood sugar levels. Reducing the intake of refined carbohydrates and sugary foods is also helpful [13].
- Physical Activity: Regular exercise increases insulin sensitivity and helps maintain a healthy weight. Engaging in at least 150 minutes of moderate-intensity aerobic activity per week is recommended.
- Weight Management: Losing excess weight is one of the most effective ways to reduce the risk of developing type 2 diabetes. A weight loss of 5-10% of body weight can significantly lower the risk [14].
- Monitoring and Support: Regular blood sugar monitoring and seeking support from healthcare professionals can aid in making sustainable lifestyle changes.
2. Dawn Phenomenon
Impact on Morning Blood Sugar Levels
The dawn phenomenon refers to an early-morning increase in blood sugar levels, typically occurring between 2 a.m. and 8 a.m. This rise in blood glucose is thought to be caused by natural hormonal changes that occur in the body during the night. Hormones such as cortisol, glucagon, and epinephrine are released, which increase insulin resistance and stimulate the liver to release more glucose into the bloodstream.
For people with diabetes, specifically those with type 1 diabetes, the dawn phenomenon can lead to high blood sugar levels upon waking. This can complicate blood sugar control and may require changes in insulin therapy or other medications to maintain target blood glucose levels. Understanding and addressing the dawn phenomenon is important for achieving optimal blood sugar control and preventing complications associated with hyperglycaemia.
Conclusion
Monitoring and managing blood sugar levels are critical components of diabetes care. Proper blood sugar control helps prevent both short-term symptoms and long-term complications associated with diabetes, such as cardiovascular disease, neuropathy, nephropathy, and retinopathy. Regular monitoring allows people to make informed decisions about their diet, physical activity, and medication, ensuring that blood glucose levels remain within target ranges. Effective management strategies, including carbohydrate control, regular exercise, and appropriate medication use, are essential for maintaining overall health and improving the quality of life for those with diabetes.
People with diabetes are encouraged to work closely with their healthcare providers to develop personalised management plans. These plans should be tailored to meet individual needs and circumstances, taking into account factors such as age, type of diabetes, lifestyle, and any existing health conditions. Regular consultations with healthcare professionals, including endocrinologists, dietitians, and diabetes educators or health coaches, can provide valuable guidance and support. By collaborating with your healthcare provider, you can achieve better blood sugar control, reduce the risk of complications, and lead healthier, more fulfilling lives.
Stay Informed & Inspired with Our Newsletter
Sign up for our newsletter to stay informed about the latest updates, episodes, helpful tips and strategies for diabetes management and holistic wellness.


