Diabetes mellitus is a chronic condition distinguished by high blood glucose levels due to the body’s inability to produce or effectively use insulin. It affects millions of people worldwide and is associated with serious complications such as cardiovascular disease, kidney failure, and neuropathy. Effective diabetes management requires maintaining blood glucose levels within a target range to prevent acute and long-term complications. Blood glucose monitoring is a critical component of diabetes management, providing essential information for making informed decisions about diet, physical activity, and medication.
Continuous Glucose Monitoring (CGM) technology significantly advances diabetes care. Unlike traditional finger-prick blood glucose testing, which provides a single snapshot of glucose levels, CGM systems continuously measure glucose levels in the interstitial fluid throughout the day and night. This continuous data stream allows for real-time monitoring and trend analysis, enabling proactive management of blood glucose levels. CGM devices typically consist of a sensor inserted under the skin, a transmitter that sends data wirelessly, and a display device such as a smartphone or dedicated monitor.
This article provides a comprehensive overview of Continuous Glucose Monitoring (CGM) technology, exploring its evolution, benefits, and future directions. It will explore the technical aspects of CGM systems, discuss the impact of CGM on diabetes management, and highlight patient experiences and challenges. In addition, the article will examine the latest innovations in CGM technology and consider concerns for users. By the end of this article, you will have a good understanding of how CGM technology is transforming diabetes care and what the future holds for this innovative approach.
Understanding Continuous Glucose Monitoring
Continuous Glucose Monitoring (CGM) is a medical technology designed to provide real-time, constant tracking of glucose levels in the body. Unlike traditional blood glucose monitoring methods that require periodic finger-prick tests, CGM systems measure glucose levels continuously throughout the day and night. This allows people with diabetes to gain a good understanding of their glucose trends and make more informed decisions about their diabetes management.
CGM systems work by measuring glucose levels in the interstitial fluid, which is the fluid surrounding the body’s cells. This method provides a near-real-time picture of glucose levels, although there is a slight delay compared to blood glucose measurements. The continuous data stream from CGM devices helps users identify patterns and trends in their glucose levels, enabling proactive management of their condition.
1. Components of a CGM System
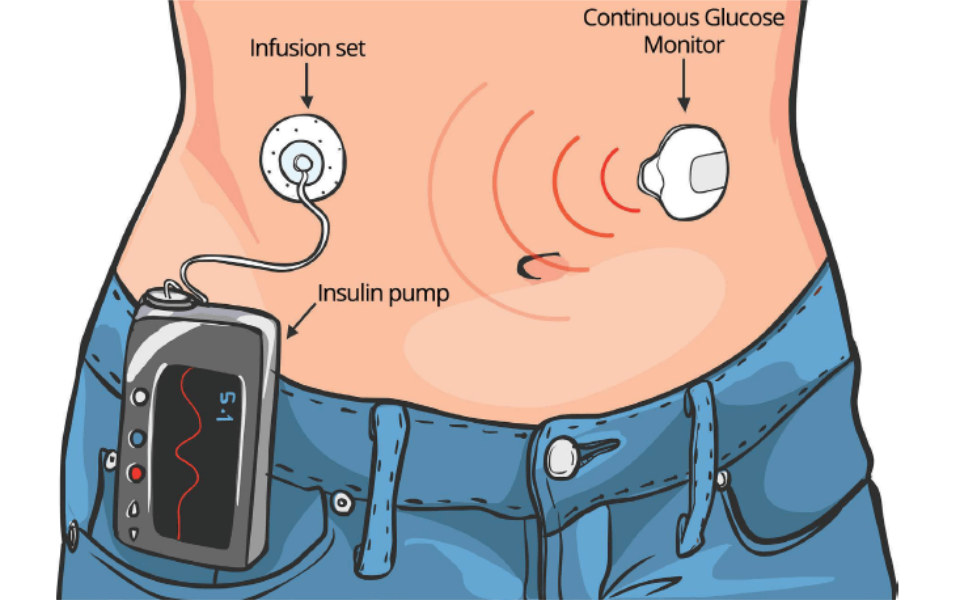
A CGM system typically consists of three main components:
1. Sensor:
- A small, disposable sensor is inserted just under the skin, usually on the belly or arm. The sensor measures glucose levels in the interstitial fluid.
- Sensors are generally waterproof and secured with an adhesive patch. They need to be replaced every 7-14 days, depending on the device.
2. Transmitter:
- The transmitter is attached to the sensor and is responsible for sending glucose readings wirelessly to the display device.
- Some CGM systems combine the sensor and transmitter into a single unit, while others have them as separate components.
3. Display Device:
- The display device can be a dedicated handheld monitor or a smartphone with a compatible app. It shows the user’s glucose levels in real time and stores historical data for trend analysis.
- The display device can also send alerts when glucose levels are too high or too low, and some systems allow data sharing with caregivers or healthcare professionals.
2. How CGM Works
CGM systems operate by continuously measuring glucose levels in the interstitial fluid. Here is a step-by-step explanation of how CGM works:
1. Measurement:
- The sensor, which contains an electrode, is inserted under the skin. It uses enzymatic technology to react with glucose molecules in the interstitial fluid, generating an electric current proportional to the glucose concentration.
- This current is then converted into a glucose reading.
2. Data Transmission:
- The transmitter attached to the sensor sends the glucose readings wirelessly to the display device at regular intervals, typically every 1 to 15 minutes.
- Some CGM systems may have a slight delay (5-20 minutes) in displaying glucose levels due to the time it takes for the glucose to travel from the bloodstream to the interstitial fluid.
3. Display and Alerts:
- The display device shows the current glucose level, trends over time, and historical data. It can also provide alerts for high or low glucose levels, helping users take timely action to manage their condition.
- Advanced CGM systems can integrate with other diabetes management tools, such as insulin pumps, to provide a more comprehensive approach to diabetes care.
By continuously monitoring glucose levels, CGM systems offer a more dynamic and detailed picture of glucose fluctuations, helping people with diabetes achieve better glycemic control and reduce the risk of complications.
Progression and Advances in CGM Technology

1. Historical Development of CGM Technology
Continuous Glucose Monitoring (CGM) technology has undergone substantial development since its inception. The first CGM systems were introduced in the early 2000s, providing intermittent glucose readings and requiring frequent calibration with finger-prick blood tests. These early devices were bulky and had limited accuracy, but they laid the groundwork for future innovations.
Over the years, CGM technology has improved dramatically in terms of accuracy, ease of use and integration with other diabetes management tools. Now modern CGM systems offer real-time glucose monitoring with minimal calibration, longer sensor wear times, and more user-friendly interfaces. These improvements have made CGM a vital tool in diabetes management, providing continuous data that helps users maintain better glycemic control and reduce the risk of complications.
2. Integration with Other Devices
One of the most significant improvements in CGM technology is its integration with other diabetes management devices, creating more comprehensive and automated systems for managing blood glucose levels.
a. Insulin Pumps:
- CGM systems can be integrated with insulin pumps to create a more seamless diabetes management experience. This integration allows for continuous glucose data to be used in adjusting insulin delivery, improving glycemic control and reducing the burden on users [1].
- Hybrid Closed-Loop (HCL) systems, also known as automated insulin delivery (AID) systems, combine CGM with insulin pumps and control algorithms to automatically adjust insulin delivery based on real-time glucose readings. These systems have shown significant benefits in maintaining glucose levels within the target range and reducing hypoglycaemia [2].
b. Connected Insulin Pens:
- Connected insulin pens (CIPs) are another innovation that integrates with CGM systems. These pens track insulin doses and timing, providing data that can be combined with CGM readings to offer a comprehensive view of glucose dynamics. This integration helps reduce missed doses and improve commitment to insulin therapy, specifically for patients using multiple daily injections (MDI) [3][4].
- CIPs often include features such as built-in bolus calculators and reminders, further enhancing their utility in diabetes management.
c. Automated Insulin Delivery (AID) Systems:
- AID systems represent the pinnacle of integrated diabetes management technology. These systems use advanced algorithms to automatically adjust insulin delivery based on continuous glucose readings from CGM devices. The goal is to mimic the natural function of the pancreas as closely as possible, providing precise and personalised insulin dosing [5].
- AID systems have been shown to improve glycemic outcomes significantly, reducing HbA1c levels and increasing the time spent within the target glucose range. They also help minimise the risk of both hyperglycaemia and hypoglycaemia, making diabetes management more effective and less burdensome.
3. Recent Technological Innovations
Recent years have seen several technological innovations that have further enhanced the capabilities and benefits of CGM systems:
a. AI-Based Decision Support:
- Artificial intelligence (AI) is increasingly being integrated into CGM systems to provide advanced decision support. AI algorithms can analyse large amounts of glucose data, predict future glucose trends, and offer personalised recommendations for insulin dosing and other management strategies.
- These AI-driven tools can help users and healthcare providers make more informed decisions, improving overall glycemic control and reducing the risk of complications.
b. Cloud-Based Data Collection:
- Cloud-based platforms allow for the seamless collection, storage, and sharing of glucose data from CGM systems. This enables users to access their data from multiple devices and share it with healthcare providers in real time.
- Cloud-based systems also facilitate remote monitoring and telemedicine, allowing for more frequent and detailed consultations with healthcare providers. This can lead to more timely interventions and better overall diabetes management.
c. Enhanced Sensor Technology:
- Advances in sensor technology have led to the development of more accurate and reliable CGM systems. Modern sensors are smaller, more comfortable to wear, and require less frequent calibration. They also offer longer wear times, reducing the need for frequent sensor replacements.
- These improvements have made CGM systems more user-friendly and accessible, increasing their adoption and effectiveness in diabetes management.
The progress and integration of CGM technology with other diabetes management tools, along with recent innovations in AI and cloud-based data collection, have significantly enhanced the capabilities and benefits of CGM systems. These innovations continue to transform diabetes care, making it more effective, personalised, and less burdensome for users.
Benefits of Continuous Glucose Monitoring

1. Improved Glycemic Control and Reduction in HbA1c Levels
One of the most significant benefits of Continuous Glucose Monitoring (CGM) is its ability to improve glycemic control. Studies have shown that CGM use is associated with a reduction in HbA1c levels, which is a key indicator of long-term blood glucose control [6][7]. By providing continuous data on glucose levels, CGM allows users to make more informed decisions about their diet, physical activity, and insulin dosing. This real-time feedback helps users maintain their glucose levels within the target range more consistently, leading to better overall glycemic control.
2. Enhanced Self-Management and Patient Empowerment
CGM empowers patients by providing them with the tools and information they need to manage their diabetes more effectively. The continuous stream of glucose data helps users understand how different factors, such as food, exercise, and stress, affect their blood glucose levels. This knowledge enables them to make proactive changes to their lifestyle and treatment plan. In addition, CGM systems often include features such as trend arrows and predictive alerts, which help users anticipate and prevent glucose excursions. This enhanced self-management capability leads to greater confidence and independence in managing diabetes.
3. Real-Time Data and Trend Analysis
The real-time data provided by CGM systems is invaluable for making timely and informed decisions about diabetes management. Unlike traditional blood glucose monitoring, which provides only sporadic snapshots of glucose levels, CGM offers a continuous and dynamic view of glucose trends. This allows users to identify patterns and trends in their glucose levels, such as the impact of specific foods or activities. With this information, users can make more precise changes to their insulin dose, meal planning, and exercise routines. The ability to analyse trends over time also helps users and healthcare providers fine-tune treatment plans for optimal outcomes.
4. Reduced Risk of Hypoglycaemia
One of the critical safety benefits of CGM is its ability to reduce the risk of hypoglycaemia, which is a dangerous condition described by abnormally low blood glucose levels. CGM systems provide real-time alerts when glucose levels are approaching dangerously low thresholds, allowing users to take immediate action to prevent hypoglycaemia. This is specifically important during activities such as exercise or sleep, when the risk of hypoglycaemia may be higher. By providing early warnings and continuous monitoring, CGM helps users maintain safer glucose levels and reduces the frequency and severity of hypoglycaemic events.
5. Reduced Complications
The long-term use of CGM has been associated with a range of health benefits and a reduction in diabetes-related complications. By maintaining better glycemic control and reducing the risk of both hyperglycaemia and hypoglycaemia, CGM helps prevent the development of complications such as cardiovascular disease, neuropathy, retinopathy, and nephropathy. Improved glucose control also contributes to better overall health and quality of life for people with diabetes. In addition, the continuous data provided by CGM can help healthcare providers make more informed decisions about treatment changes, leading to better long-term outcomes.
Continuous Glucose Monitoring offers numerous benefits, including improved glycemic control, enhanced self-management, real-time data for better decision-making, increased safety, and long-term health benefits. These advantages make CGM an essential tool in the effective management of diabetes, helping users achieve better health outcomes and a higher quality of life.
Patient Experiences and Challenges
1. Positive Patient Experiences
a. Convenience:
- Many patients find CGM systems to be highly convenient compared to traditional finger-prick methods. Continuously monitoring glucose levels without requiring frequent manual testing simplifies daily diabetes management. Users appreciate the ease of checking their glucose levels at any time, without additional equipment or procedures.
b. Reassurance:
- CGM provides a sense of reassurance by offering real-time data and alerts. Patients feel more secure knowing they will be alerted to any significant changes in their glucose levels, allowing them to take immediate action if necessary. This continuous monitoring helps reduce anxiety about potential hypoglycaemic or hyperglycaemic events, especially during sleep or physical activity.
c. Motivation:
- Detailed feedback from CGM systems can be highly motivating for patients. Seeing the direct impact of their lifestyle choices on their glucose levels encourages them to make healthier decisions. The ability to track progress over time and see improvements in glycemic control can boost motivation and commitment to treatment plans.
2. Common Challenges and Barriers
a. Device Complexity:
- Some patients find CGM systems complex and challenging to use, specifically those who are not tech-savvy. The initial setup, calibration, and interpretation of data can be daunting for new users. In addition, managing the various components (sensor, transmitter, display device) and ensuring they work together seamlessly can be frustrating.
b. Cost:
- The cost of CGM systems can be a significant barrier for many patients. While some insurance plans cover CGM devices, others do not, leaving patients to bear the full cost out-of-pocket. The expense of sensors, which need to be replaced regularly, adds to the overall cost. This financial burden can make CGM inaccessible for some people, specifically those without inclusive health insurance.
c. Discomfort:
- Inserting the sensor can cause discomfort or pain for some users. Although modern sensors are designed to be as minimally invasive as possible, the insertion process and wearing the sensor for extended periods can still be uncomfortable. Skin irritation or allergic reactions to the adhesive used to secure the sensor are also common complaints.
3. Importance of Education and Training for Effective Use
a. Education:
- Proper education is crucial for the effective use of CGM systems. Patients need to understand how to set up and calibrate their devices, interpret the data, and respond to alerts. Comprehensive education programs can help demystify the technology and build confidence in using CGM. This education should cover not only the technical aspects but also how to integrate CGM data into daily diabetes management.
b. Training:
- Hands-on training is essential to ensure patients can use their CGM systems effectively. Training sessions can include practical demonstrations, troubleshooting tips, and personalised guidance based on the patient’s unique needs and lifestyle.
c. Ongoing Support:
- Continuous support from healthcare providers is vital for long-term success with CGM. Regular follow-up appointments can help address any issues, adjust treatment plans based on CGM data, and provide encouragement and motivation. Access to a support network, whether through healthcare providers, diabetes educators, or peer support groups, can also enhance the patient experience and improve outcomes.
While Continuous Glucose Monitoring offers numerous benefits and positive experiences for patients, it also presents challenges such as device complexity, cost, and discomfort. Education and training are critical to overcoming these barriers and ensuring that patients can effectively use CGM technology to manage their diabetes.
User Experience and Design Considerations

1. Importance of User-Centred Design in CGM Systems
User-centred design is crucial in developing Continuous Glucose Monitoring (CGM) systems to ensure that they meet the needs and preferences of end-users. CGM devices are not just medical tools but an integral part of a person’s daily life, requiring seamless integration into their routines and activities. A user-centred approach involves actively engaging users throughout the design process, gathering insights into their experiences, challenges, and expectations [8].
By involving users from the early stages of design, developers can better understand the real-world contexts in which CGM systems are used. This includes factors such as usability, accessibility, and the emotional impact of living with a health condition like diabetes. User-centred design helps identify potential pain points, usability issues, and areas for improvement, leading to more intuitive and user-friendly CGM systems.
2. Key User Needs and Preferences
Through user research and feedback, several key user needs and preferences have emerged for CGM systems:
a. Ease of Use:
- Users desire CGM systems that are simple and intuitive to set up, operate, and maintain. Clear instructions, straightforward navigation, and minimal complexity are essential for ensuring a positive user experience [9].
- Streamlining tasks like sensor insertion, data interpretation, and alert management can significantly improve user satisfaction and commitment.
b. Clear Navigation and Visual Data:
- Effective navigation and visual data are critical for users to understand and act upon their glucose data. Clear and intuitive interfaces, with well-organised information and meaningful visualisations, can help users quickly grasp trends and patterns [10].
- Customisable displays and the ability to filter or highlight specific data points can further enhance the user experience.
c. Integrated Systems:
- Many users express a preference for integrated systems that combine CGM functionality with other diabetes management tools, such as insulin pumps, bolus calculators, and activity trackers.
- A “system of systems” approach, where different components seamlessly communicate and share data, can simplify diabetes management and reduce the burden on users.
d. Personalised and Customisable Systems:
- Users have different needs, preferences, and lifestyles. The ability to personalise CGM systems, such as customising alerts, setting individual goals, and tailoring data displays, can enhance user engagement and satisfaction [11].
e. Discreet and Comfortable to Wear:
- Users appreciate CGM systems that are discreet, comfortable to wear, and minimally intrusive in their daily activities. Factors like sensor size, adhesive quality, and wearable design can significantly impact user experience.
3. Case Studies and Feedback from End Users
Several studies and user feedback sessions have provided valuable insights into the user experience of CGM systems:
a. Dexcom G7 Usability Study [9]:
- This study evaluated the ease of use and teachability of the Dexcom G7 CGM system among certified diabetes care and education specialists (CDCESs) and CGM-naïve older adults with type 2 diabetes.
- Participants provided feedback on the setup process, sensor insertion, and overall usability. The study highlighted the importance of clear instructions, intuitive design, and user training for successful adoption.
b. User Experience Study on CGM Systems [1]:
- This study explored the user experience of CGM systems through interviews and surveys with end-users in Sweden.
- Participants expressed a desire for improved navigation, better integration with other systems, and more personalised features. The study led to the development of a prototype CGM system with enhanced user experience.
c. Co-creation Design Process for T2D Solutions [10]:
- Researchers from the Technical University of Denmark conducted a co-creation design process involving users with type 2 diabetes.
- Participants provided insights into their needs and preferences, leading to the development of prototypes for an activity-based CGM app and a personalised diabetes guide.
- The prototypes emphasised the importance of flexible, personalised systems and positively framed content to encourage user engagement.
d. CGM App Design Considerations [11]:
- This article discusses the design considerations for a CGM app, highlighting the importance of user-centred design and addressing key user needs.
- It emphasises the need for clear visual data, personalisation options, and seamless integration with other diabetes management tools.
These case studies and user feedback sessions underscore the importance of involving end-users throughout the design process of CGM systems. By addressing their needs and preferences, developers can create more user-friendly, engaging, and effective CGM solutions, ultimately improving diabetes management and quality of life for users.
Future Directions and Innovations
1. Emerging Technologies in CGM
a. Automated Insulin Delivery (AID) Systems
One of the most promising future directions in CGM technology is the development of fully automatic Automated Insulin Delivery (AID) systems, also known as closed-loop systems or artificial pancreas systems. These systems integrate CGM with insulin pumps and advanced control algorithms to automatically adjust insulin delivery based on real-time glucose readings, mimicking the function of a healthy pancreas [12].
While current hybrid closed-loop systems still require some user input, such as announcing meal intake, fully automatic AID systems aim to eliminate the need for manual intervention. These systems will use advanced algorithms and machine learning techniques to predict glucose trends, calculate insulin requirements, and automatically deliver the appropriate insulin doses.
Fully automatic AID systems have the potential to significantly improve glycemic control, reduce the risk of hypoglycaemia and hyperglycaemia, and alleviate the burden of diabetes management for users [13].
b. AI-Driven Tools and Decision Support
Artificial Intelligence (AI) is increasingly integrated into CGM systems and diabetes management platforms. AI algorithms can analyse large amounts of glucose data, identify patterns, and provide personalised recommendations for insulin dose, diet, and physical activity [14].
AI-driven decision support tools can assist users and healthcare providers make more informed and timely decisions, leading to better glycemic outcomes. These tools can also help predict and prevent potential glucose excursions, reducing the risk of complications.
In addition, AI can be used to optimise insulin delivery algorithms in AID systems, further improving their accuracy and effectiveness.
2. Advances in Biosensors and Wearable Technology
Continuous improvements in biosensor technology are driving the development of more accurate, reliable, and user-friendly CGM systems. Researchers are exploring new sensing materials, enzymes, and detection methods to improve sensor performance and extend sensor life [15].
One area of focus is the development of non-invasive or minimally invasive glucose monitoring techniques. These include optical sensors that measure glucose levels through the skin using infrared or Raman spectroscopy, as well as sensors that analyse glucose in biofluids such as tears, sweat, or saliva.
In addition, the integration of CGM technology into wearable devices, such as smartwatches or fitness trackers, is an emerging trend. These wearable CGM systems can provide seamless and discreet glucose monitoring, improving user convenience and commitment [16].
3. Potential Future Developments and Impact
The future of CGM technology holds immense potential for transforming diabetes management. Some potential developments and their impact include:
- Improved Glycemic Control and Reduced Complications: With fully automatic AID systems, AI-driven decision support, and advanced biosensors, people with diabetes may achieve unprecedented levels of glycemic control. This could significantly reduce the risk of long-term complications, such as cardiovascular disease, neuropathy, and retinopathy.
- Enhanced Quality of Life: The integration of CGM into wearable devices and the automation of insulin delivery could alleviate the burden of diabetes management, allowing individuals to focus on living their lives without constant monitoring and changes.
- Remote Monitoring and Telemedicine: Cloud-based data collection and sharing capabilities could enable remote monitoring of glucose levels by healthcare providers, facilitating timely interventions and reducing the need for frequent in-person visits.
- Personalised and Precision Diabetes Care: AI-driven tools and the analysis of large datasets could lead to personalised treatment plans tailored to individual needs, taking into account factors such as genetics, lifestyle, and comorbidities.
- Improved Access and Affordability: Advances in sensor technology and manufacturing processes could potentially reduce the cost of CGM systems, making them more accessible to a wider population.
The future of CGM technology holds immense promise for revolutionising diabetes management, improving health outcomes, and enhancing the quality of life for people living with this health condition.
Practical Considerations for CGM Users

1. How to Choose the Right CGM System
Selecting the appropriate Continuous Glucose Monitoring (CGM) system is crucial for ensuring optimal diabetes management and user satisfaction. Here are some key factors to consider when choosing a CGM system:
- Accuracy: Look for CGM systems with high accuracy ratings, as this ensures reliable glucose readings and better decision-making. Review clinical studies and accuracy reports from independent organisations [17].
- Sensor Wear Time: Different CGM systems offer varying sensor wear times, ranging from 7 to 14 days or more. Consider your lifestyle and preferences when choosing a system with a suitable wear time.
- Integration: If you use an insulin pump or other diabetes management devices, consider a CGM system that integrates seamlessly with those devices. Integrated systems can provide a more comprehensive and convenient solution [18].
- User Interface: Evaluate the user interface of the CGM system, including the display device, mobile app, and data visualisation. Choose a system that is intuitive, easy to navigate, and aligns with your preferences [19].
- Alerts and Alarms: Consider the customisation options for alerts and alarms, such as high and low glucose thresholds, rate of change alerts, and predictive alerts. Ensure the system offers flexibility to tailor alerts to your needs.
- Data Sharing: If you plan to share your CGM data with healthcare providers or caregivers, look for systems that offer secure data sharing and remote monitoring capabilities.
- Cost and Insurance Coverage: Evaluate the overall cost of the CGM system, including the initial purchase, ongoing sensor and transmitter costs, and any associated subscription fees. Check with your insurance provider for coverage details.
2. Tips for Effective Use and Maintenance
To maximise the benefits of your CGM system and ensure accurate and reliable performance, follow these tips:
- Proper Sensor Insertion: Follow the manufacturer’s instructions carefully for sensor insertion and site rotation. Proper insertion and site selection can improve sensor accuracy and reduce discomfort [20].
- Calibration: If your CGM system requires calibration, ensure that you calibrate it as per the manufacturer’s guidelines. Use fresh, unexpired test strips and follow proper hand-washing and finger-pricking techniques.
- Skin Preparation: Clean and dry the insertion site thoroughly before the sensor application. Consider using skin preparation products recommended by the manufacturer to improve connection and reduce irritation.
- Monitoring and Troubleshooting: Regularly check your CGM system for proper functioning, and address any issues promptly. Refer to the user manual or contact the manufacturer’s support for troubleshooting guidance.
- Data Interpretation: Understand how to interpret the CGM data, including trend arrows, rate of change, and glucose patterns. Consult with your healthcare provider or a diabetes educator for guidance.
- Lifestyle Integration: Incorporate your CGM data into your daily routine, making changes to your diet, exercise, and medication as needed based on the real-time glucose information.
3. Addressing Common Issues and Troubleshooting
Despite their advanced technology, CGM systems can sometimes encounter issues or challenges. Here are some common problems and troubleshooting tips:
- Sensor Inaccuracy or Dropouts: If you notice inaccurate readings or frequent signal dropouts, check the sensor insertion site for proper connection, moisture, or compression. Consider replacing the sensor if the issue persists.
- Skin Irritation or Rashes: Some users may experience skin irritation or rashes at the sensor insertion site. Try rotating insertion sites, using skin preparation products, or consulting your healthcare provider for alternative solutions.
- Interference or Compression Artifacts: Certain medications (e.g., acetaminophen), compression on the sensor site (e.g., sleeping on the sensor), or electromagnetic interference can affect CGM readings. Refer to the user manual or contact the manufacturer for guidance on addressing these issues.
- Battery or Connectivity Issues: Ensure that the CGM system components (transmitter, display device, etc.) are properly charged and connected. Follow the manufacturer’s instructions for troubleshooting connectivity or battery-related problems.
- Data Sharing or Uploading Issues: If you encounter difficulties sharing or uploading your CGM data, check your internet connection, ensure data sharing is enabled, and see the manufacturer’s support resources.
By considering these practical considerations, choosing the right CGM system, following best practices for effective use and maintenance, and addressing common issues promptly, you can optimise the benefits of CGM technology and achieve better glycemic control and overall diabetes management.
Conclusion
Continuous Glucose Monitoring (CGM) technology has revolutionised diabetes management by providing real-time, continuous tracking of glucose levels. The key benefits of CGM include:
- Improved glycemic control and reduction in HbA1c levels
- Enhanced self-management through real-time data
- Increased safety and reduced risk of hypoglycaemia with predictive alerts
- Long-term health benefits and reduced complications from better glucose management
CGM technology has the potential to transform diabetes management by providing unprecedented levels of glycemic control and reducing the burden of self-management. The integration of CGM with AID systems, also known as artificial pancreas systems, can automate insulin delivery, mimicking the function of a healthy pancreas. This automation can significantly improve the quality of life for people with diabetes, allowing them to focus on living their lives without constant monitoring and adjustments.
Furthermore, the integration of CGM data with AI-driven decision support tools and virtual platforms can enable personalised and precision diabetes care. These systems can analyse large datasets, identify patterns, and provide tailored recommendations for insulin dose, diet, and physical activity, leading to better long-term outcomes.
The future of CGM technology holds immense promise for revolutionising diabetes management. Improvements in biosensor technology, wearable devices, and non-invasive or minimally invasive glucose monitoring techniques are expected to make CGM systems more accurate, reliable, and user-friendly.
In addition, the integration of CGM data with cloud-based platforms and remote monitoring capabilities can facilitate telemedicine and enable healthcare providers to make timely interventions, reducing the need for frequent in-person visits.
As CGM technology continues to evolve, it has the potential to become more accessible and affordable, enabling a wider range of people with diabetes to benefit from its advantages. The ultimate vision is an integrated, cloud-based environment that connects, monitors, and informs people with diabetes, empowering them to independently manage and treat this health condition effectively.
While challenges remain, such as cost and insurance coverage barriers, the transformative potential of CGM technology in improving health outcomes, reducing complications, and enhancing the quality of life for people with diabetes is undeniable. As research and development continue, CGM is poised to play a vital role in the future of diabetes management, offering a more personalised, efficient, and empowering approach to this condition.
Stay Informed & Inspired with Our Newsletter
Sign up for our newsletter to stay informed about the latest updates, episodes, helpful tips and strategies for diabetes management and holistic wellness.


